Building LGBTQ+ Families Through Reciprocal IVF
For many LGBTQ+ couples, the path to parenthood is a journey of intention, research, and love. Reciprocal In Vitro Fertilization (Reciprocal IVF), also known as co-IVF or the ROPA method, has emerged as a profoundly meaningful option for lesbian couples and transgender men, allowing both partners in a same-sex female couple to participate biologically in the creation of their family. Unlike conventional assisted reproductive technology, this process allows one partner to provide the eggs (the genetic mother) while the other carries the pregnancy and gives birth (the gestational mother). It’s a process that beautifully intertwines genetics and gestation, creating a unique connection for both mothers and their child from the very beginning. However, this journey is often accompanied by complex questions about the process, its costs, navigating insurance coverage, and understanding realistic success rates based on current research and data.
Welcome to Shared Motherhood and Co-Maternity
Reciprocal IVF is more than a medical procedure; it represents a powerful form of shared motherhood. One partner provides the genetic contribution through egg retrieval, while the other partner becomes the gestational mother, carrying the pregnancy to term. This concept of co-maternity is a powerful way for both individuals to have a distinct and vital biological role in building their family, fostering a deep sense of shared parenthood from conception. This method creates a unique family dynamic where both partners are biologically connected to their child in different but equally meaningful ways.
What Is Reciprocal IVF (Co-IVF) and Why Is It for LGBTQ+ Families?
This specialized form of In Vitro Fertilization (IVF) is designed primarily for couples with two uteruses—including cisgender lesbian couples, couples involving a transgender man who can provide eggs, and others in the LGBTQIA+ community seeking to build a family together. Unlike traditional fertility treatments where one person might undergo the entire process, reciprocal IVF splits the key roles between both partners. This dual involvement is its primary appeal, offering a unique path to family-building through shared motherhood that honors both partners’ desire to be physically connected to their child’s creation.
What This Guide Covers: Costs, Coverage, Success, and Beyond
Navigating the world of fertility treatments can be overwhelming. This guide is designed to provide a clear, comprehensive overview of Reciprocal IVF for LGBTQ+ families. We will demystify the entire process, from the initial consultation to the final embryo transfer. More importantly, we will provide a transparent breakdown of the associated costs, offer strategies for navigating complex insurance coverage, and set realistic expectations by explaining success rates and the factors that influence them. Throughout this guide, you’ll find information about leading clinics like CNY Fertility and Pacific Fertility Center Los Angeles, as well as guidance from major reproductive health organizations.
Understanding Reciprocal IVF (Co-IVF): The Basics
At its core, Reciprocal IVF is a collaborative approach to building a family that leverages established assisted reproductive technology in a way that is uniquely suited for same-sex female couples and others in the LGBTQ+ community.
Defining Reciprocal IVF: Shared Biological Parenthood
Reciprocal IVF is a variation of standard In Vitro Fertilization where eggs are retrieved from one partner through a procedure called egg retrieval, fertilized in a laboratory with donor sperm to create embryos, and then one of those embryos is transferred into the other partner’s uterus to carry the pregnancy. This method results in one partner being the genetic mother (the egg donor) and the other being the gestational mother, who gives birth. It is a powerful affirmation of shared parenthood and allows the LGBTQIA+ community to experience family-building in a deeply personal way.
The Roles of Partner A (Genetic Mother) and Partner B (Gestational Carrier)
The process involves two distinct but equally important roles:
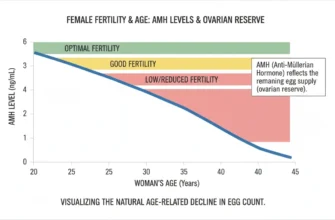
Partner A (Genetic/Egg Donor Mother): This partner undergoes ovarian stimulation with fertility medications to produce multiple mature eggs. She then has an egg retrieval procedure, also known as oocyte retrieval. Her age and ovarian reserve (measured through Anti-Müllerian hormone testing) are primary factors in the potential success of the cycle. Antral follicles count (AFC) and baseline hormone levels provide critical information about egg quantity and quality.
Partner B (Gestational Mother/Carrier): This partner prepares her uterus to receive the embryo. She takes medications to thicken her uterine lining and, following embryo transfer, carries the pregnancy. Her uterine health is a key factor for successful implantation and a healthy pregnancy. Partner B must also have healthy fallopian tubes (if relevant to clinic protocols) and no significant uterine abnormalities.
How Reciprocal IVF Differs from Conventional IVF for Same-Sex Couples
In conventional IVF for a same-sex couple, one partner would typically provide the eggs and carry the pregnancy. The key difference in Reciprocal IVF is the intentional separation of these roles. This requires medical evaluation and cycle synchronization for both partners, making it a more complex and often more expensive process than standard IVF, but one that many couples find deeply rewarding. Both partners are treated as patients throughout the process, with separate consultations, testing, and monitoring.
The Reciprocal IVF Journey: A Step-by-Step Guide
The Reciprocal IVF process is a carefully orchestrated medical journey that involves both partners in distinct, synchronized phases. Each step is managed by a specialized fertility clinic with expertise in assisted reproductive technology.
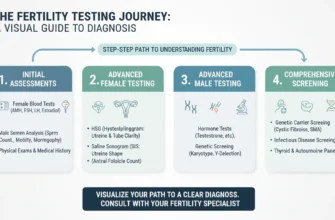
Initial Consultations and Pre-Cycle Testing
The journey begins with consultations with a reproductive endocrinologist. Both partners undergo a comprehensive fertility evaluation. Partner A’s testing focuses on ovarian reserve (egg quantity and quality), including blood work to measure Anti-Müllerian hormone (AMH), follicle-stimulating hormone (FSH), and estradiol levels, as well as a transvaginal ultrasound to assess antral follicles count (AFC). Infectious disease testing for Hepatitis B, Hepatitis C, HIV, and other pathogens is also required.
Partner B’s evaluation centers on uterine health and the ability to carry a pregnancy. This includes a hysterosalpingogram (HSG) or sonohysterogram to assess uterine structure, hormone levels, and sometimes an endometrial receptivity assessment. This phase also includes selecting donor sperm from a reputable sperm bank. Couples should review the sperm donor profiles carefully, considering health history, genetic screening, and whether they want an ID-release or non-ID-release donor.
Ovarian Stimulation and Egg Retrieval for Partner A
Partner A begins a course of injectable fertility medications (gonadotropins) to stimulate her ovaries to produce multiple eggs. This process, known as ovarian stimulation, is monitored closely with blood tests and ultrasound appointments. The stimulation typically lasts 8-14 days, during which hormone levels are tracked to optimize embryo development. Once the eggs are mature, she undergoes a minor surgical procedure called egg retrieval, where a physician retrieves the eggs from her ovaries using a needle guided by ultrasound. This procedure typically takes 15-20 minutes and is performed under light sedation or anesthesia. The number and quality of eggs retrieved directly impact the success potential of the cycle.
Fertilization, Embryo Development, and Optional Genetic Testing
The retrieved eggs are then fertilized in the lab with the chosen donor sperm. This may be done through conventional insemination or via Intracytoplasmic Sperm Injection (ICSI), where a single sperm is injected directly into each egg. The resulting embryos are cultured for several days, typically reaching the blastocyst stage by day 5. Embryo development is carefully monitored, with daily assessments of cell division and morphology.
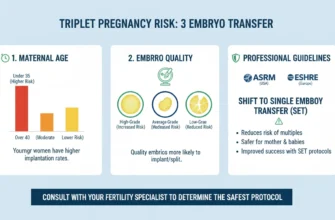
During this time, couples may opt for Preimplantation Genetic Testing (PGT) to screen embryos for chromosomal abnormalities, potentially increasing the chances of a successful pregnancy. Genetic testing can identify genetic abnormalities and help select the healthiest embryos for transfer. AI Embryo Monitoring technology is increasingly being used by leading clinics to assess embryo health and predict which embryos have the highest implantation potential. Blastocysts are graded using the Gardner grading system, which assesses expansion stage, inner cell mass (ICM) quality, and trophectoderm (TE) quality. Higher-grade embryos (such as 5AA or 5AB) typically have higher success rates.
Embryo Transfer for Partner B and Early Pregnancy
While Partner A is undergoing stimulation, Partner B takes hormones (estrogen and progesterone) to prepare her uterine lining for implantation. When the lining is receptive, the best-quality embryo is transferred into her uterus in a simple, non-surgical procedure called single embryo transfer, though some couples may elect multiple embryo transfer depending on circumstances and clinic protocols. A pregnancy test is typically performed about 9-14 days after the embryo transfer. Any remaining viable embryos can be frozen through embryo freezing and embryo cryopreservation for a future frozen embryo transfer (FET).
Demystifying Reciprocal IVF Costs for LGBTQ+ Families
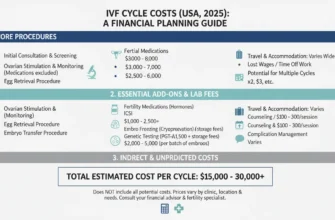
Financial planning is one of the most significant aspects of the Reciprocal IVF journey. Costs can vary widely based on the fertility clinic, location, and the specific medical needs of the couple. As of 2025, costs have remained relatively stable compared to 2024, though expenses continue to rise due to advanced technology and increased demand.
Breaking Down the Base Cost of a Reciprocal IVF Cycle
The base cost of a single Reciprocal IVF cycle typically ranges from $20,000 to $35,000+ per cycle. This fee generally covers the core medical procedures for both partners, including:
-
Cycle management and monitoring for both partners (ultrasound scans and bloodwork)
-
Anesthesia fees for the egg retrieval procedure (often $500-$1,000, sometimes separate)
-
The egg retrieval procedure for Partner A
-
Laboratory fees for fertilization and embryo culture
-
The embryo transfer procedure for Partner B
-
Initial embryo monitoring and grading
Essential Add-on Costs That Impact the Total
Beyond the base cycle fee, several necessary costs significantly increase the total investment.
Fertility Medications: Ovarian stimulation drugs for Partner A and uterine preparation medications (hormone injections for Partner B) can cost between $3,000 and $8,000. Medication costs vary depending on the stimulation protocol, dosage, and pharmacy. Shopping around and using prescription assistance programs can reduce this cost.
Donor Sperm: Purchasing vials of sperm from a sperm bank typically costs $800 to $3,000+ per vial, plus shipping and storage fees. Most reciprocal IVF cycles use 2-4 vials. Couples should budget for multiple vials in case the first batch doesn’t result in fertilization or pregnancy.
Genetic Testing (PGT): If chosen, Preimplantation Genetic Testing can add $3,000 to $7,000 to the total, though it may improve success rates by identifying the healthiest embryos. AI Embryo Monitoring technology costs vary by clinic but typically add $500-$2,000.
Embryo Freezing and Storage: Initial embryo freezing and the first year of storage can cost $1,000 to $2,000, with annual storage fees thereafter (typically $300-$500/year for continued storage).
Laboratory Add-ons: Additional services such as ICSI (embryonic procedure) can cost $1,000-$2,500. Advanced services like time-lapse imaging or assisted hatching may add $500-$1,500 each.
Legal Consultation: Legal fees for reproductive contracts, donor agreements, and ensuring both partners’ parental rights are protected typically range from $1,500-$3,000.
Indirect and Often Overlooked Expenses
Couples should also budget for indirect costs. These can include:
-
Travel and accommodation if the chosen fertility clinic is not local
-
Time off work for appointments (often 15-20 appointments per cycle)
-
Costs for legal consultations to establish legal parenthood for both partners
-
Psychological counseling and support services
-
Medications for side effects or complications
-
Repeat cycles (many couples budget for 2-3 cycles)
Estimating Your Investment: Using Cost Calculators and Transparent Pricing
Many fertility clinics offer financial counseling and transparent pricing lists. Leading clinics like CNY Fertility and Pacific Fertility Center Los Angeles provide detailed breakdowns of costs. Don’t hesitate to ask for a detailed, itemized cost estimate that includes all potential add-ons. Some clinics also provide online cost calculator tools to help you build a preliminary budget for your specific fertility treatments.
A realistic total investment for a couple pursuing Reciprocal IVF should include $50,000-$70,000 when accounting for medications, sperm, testing, and a realistic pathway to achieving pregnancy.
Navigating Insurance Coverage and Financial Support
Insurance coverage for fertility treatments is a complex and often frustrating landscape, particularly for LGBTQ+ couples. Understanding your benefits and advocating for yourself is critical. The landscape is improving significantly as of 2024-2025, with more inclusive definitions and expanded coverage.
Understanding Your Fertility Insurance Benefits
Many insurance plans still use outdated definitions of infertility that require a heterosexual couple to have unprotected intercourse for six to twelve months without conceiving. This definition effectively excludes same-sex couples from coverage. However, advocacy is changing this landscape, and many progressive employers and insurers have updated their policies.
As of 2025, 21 states plus Washington D.C. have laws mandating fertility insurance coverage. Key states with inclusive mandates include:
-
Maryland (first state to include same-sex couples, 2015)
-
New Jersey (2017)
-
New York (2020 – updated to FAFTA, covers egg freezing and multiple IVF cycles)
-
Illinois (2022 – inclusive language)
-
California (SB 729 – effective 2026, covers up to 3 egg retrievals and unlimited embryo transfers)
Scrutinize your policy for language related to “fertility treatments” or “assisted reproductive technology” and ask your HR department for a complete Summary of Benefits and Coverage.
Specific Programs and Providers: Progyny, Carrot, WINFertility, and Beyond
A growing number of employers are offering more inclusive fertility benefits through specialized providers. Progyny is one of the largest vendors, counting Reciprocal IVF as 1.25 cycles (reflecting the extra complexity of treating two patients). Carrot Fertility offers flexible, bundled and à la carte options with strong LGBTQ+ support. WINFertility (WIN) specifically serves the LGBTQIA+ community with dedicated care advocates and 1:1 financial coaching. All three providers cover:
-
Reciprocal IVF and other fertility treatments
-
Donor sperm and donor egg services
-
Embryo freezing and storage
-
Psychological support
-
Adoption and surrogacy services
Each provider operates on a different model, so discussing your specific needs with your employer’s benefits team is essential.
State Insurance Mandates and LGBTQ+ Coverage
According to RESOLVE and the Kaiser Family Foundation, as of September 2024:
-
21 states plus D.C. have fertility insurance mandates
-
15 states include IVF coverage
-
17 states cover fertility preservation
-
Only a subset explicitly include same-sex couples or have eliminated the “unprotected intercourse” requirement
States like New York, Illinois, and Maryland have the most inclusive language that explicitly benefits LGBTQ+ families. Texas and California require insurers to offer coverage, but employers don’t have to select plans that include it.
Strategies for Appealing Denials and Seeking Financial Assistance
If your claim is denied, file an appeal. A letter from your reproductive endocrinologist explaining the medical necessity of Reciprocal IVF can be powerful. Look into grants from organizations like Family Equality’s Path to Parenthood or the Tinina Q. Cade Foundation. Many fertility clinics also offer in-house financing plans, multi-cycle discount packages, or shared-risk programs. Additionally, consider:
-
Maximizing FSA/HSA accounts (up to $3,050/year for 2025)
-
Seeking grants from LGBTQ+ organizations
-
Exploring fertility-specific lenders offering 0% financing
-
Discussing payment plans directly with your clinic
Reciprocal IVF Success Rates Explained: Realistic Expectations
Success rates in any IVF cycle are never guaranteed. Understanding the statistics and the factors that influence them can help you manage emotional and financial expectations.
General IVF Success Rates for LGBTQ+ Families
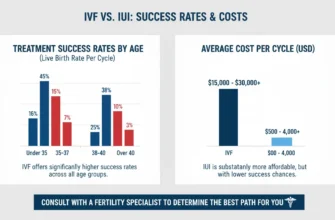
Success rates for Reciprocal IVF are comparable to those of traditional IVF and are largely dependent on the age of the partner providing the eggs. Because many LGBTQ+ couples pursuing IVF do not have an underlying infertility diagnosis, their success rates can sometimes be higher than the general population average. Data from the Centers for Disease Control and Prevention (CDC) and Society for Assisted Reproductive Technology (SART) provide national averages based on age.
IVF Success Rates by Age of Egg Provider
Based on 2023-2024 data from the American Society for Reproductive Medicine (ASRM) and CDC reports:
Women Under 35: Live birth rate of 41-55% per cycle. Clinical pregnancy rates may reach 50%+. These younger patients typically have the highest egg quality and quantity.
Women 35-37: Live birth rate of 30-41% per cycle. Clinical pregnancy rates average 35-40%. Egg quality begins to decline, but outcomes remain favorable.
Women 38-40: Live birth rate of 20-27% per cycle. Clinical pregnancy rates drop to 25-30%. Chromosomal abnormalities become more common.
Women Over 40: Live birth rate of approximately 7-10% per cycle. Only about 5% for women over 42. Miscarriage rates increase significantly due to genetic abnormalities.
Key Factors Influencing Your Chances of Success
Several critical factors determine the likelihood of a live birth:
Age of the Egg Provider: This is the single most important factor. Egg quality and quantity decline significantly after age 35, with a more dramatic decline after age 38. The age of the egg donor (even if that donor is your partner) is the strongest predictor of success rates.
Embryo Quality: The health of the embryos created is paramount. Genetic testing (PGT) can help select the most viable embryo. Embryos graded as 5AA or 5AB have the highest implantation potential, while lower grades (3BC, 4BC) have significantly reduced success rates.
Uterine Health of the Carrier: The partner carrying the pregnancy must have a healthy, receptive uterus. The endometrial thickness should be 7-14mm at the time of transfer. Uterine abnormalities or poor endometrial receptivity can reduce implantation rates.
Fertility Clinic Expertise: The experience and laboratory quality of your chosen fertility clinic play a significant role. Clinics like CNY Fertility and Pacific Fertility Center Los Angeles with dedicated LGBTQ+ programs typically have higher success rates due to specialized expertise and advanced technology like AI Embryo Monitoring.
Lifestyle Factors: The health of both partners, including weight, smoking, alcohol use, and stress levels, can impact outcomes. Maintaining a healthy BMI (18.5-24.9) and avoiding smoking and excessive alcohol improve success rates.
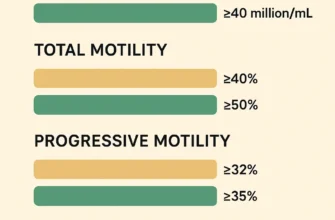
Donor Sperm Quality: The quality and motility of the sperm sample used for fertilization affects fertilization rates and embryo development. Reputable sperm banks screen for motility, morphology, and genetic health.
Cumulative Success Rates Across Multiple Cycles
While single-cycle success rates vary by age, cumulative success rates improve significantly with multiple cycles:
-
Under 35: 60-80% cumulative live birth rate after 2-3 cycles
-
35-37: 50-70% cumulative live birth rate after 2-3 cycles
-
38-40: 35-55% cumulative live birth rate after 2-3 cycles
-
Over 40: 15-35% cumulative live birth rate after multiple cycles
This is why many couples budget for 2-3 cycles from the start, even if they achieve success on the first try.
Setting Realistic Expectations and Preparing Emotionally
It’s important to remember that it may take more than one cycle to achieve a successful pregnancy. A failed cycle is emotionally and financially devastating. Building a strong support system, including a therapist specializing in fertility, can be invaluable. Discussing possibilities like using a different partner’s eggs (switching roles for a second child) or pursuing a frozen embryo transfer can prepare you for future decisions.
Additionally, be aware of potential health complications specific to reciprocal IVF and donor egg pregnancies. Recent research from 2024-2025 shows:
-
Hypertensive disorders (pre-eclampsia) occur in 23.8% of co-IVF pregnancies vs. 12.9% in heterosexual own-egg IVF
-
Gestational diabetes affects 9.5% of co-IVF pregnancies vs. 1.6% in own-egg IVF
-
Preterm birth and lower birthweight are more common
-
These complications are not well-understood but may relate to genetic abnormalities or maternal-fetal immunological factors
Partner B should be counseled about these increased risks and monitored closely throughout pregnancy.
Legal and Ethical Considerations for LGBTQ+ Parents
The legal framework surrounding assisted reproduction for LGBTQ+ families is crucial to protect both partners’ parental rights.
Establishing Legal Parenthood for Both Partners
Even if both partners are on the birth certificate, it is highly recommended that the non-biological mother (Partner B, the gestational mother, in many states’ legal frameworks) complete a second-parent adoption or stepparent adoption. This process legally severs ties with the sperm donor and solidifies the parental rights of the non-genetic mother, ensuring her legal relationship with the child is protected regardless of where you live or travel.
State laws vary significantly. Some states automatically recognize both parents if they’re married at the time of birth. Others require explicit documentation. Arkansas and Oklahoma have been particularly resistant to recognizing same-sex parents on birth certificates. Second-parent adoption eliminates this uncertainty and should be pursued even in progressive jurisdictions, as it provides the strongest legal protection.
This is especially important given the potential for relationship changes. If the couple separates or divorces, a second-parent adoption ensures that both partners have established parental rights and can seek custody or visitation rights if appropriate.
Decision-Making for Embryos: Present and Future
Before starting the cycle, couples must make legally binding decisions about what to do with any remaining frozen embryos in the event of separation, divorce, or death. These decisions are complex but essential for protecting both partners’ future reproductive choices. Consulting with a lawyer specializing in reproductive law is a critical step in the Reciprocal IVF process.
Specific questions to address include:
-
What happens to frozen embryos if one partner dies?
-
What happens to frozen embryos if the couple divorces?
-
Can one partner use a frozen embryo without the other’s consent?
-
What is the financial responsibility for continued storage?
-
Should embryos be donated to research or other couples if neither partner uses them?
A donor conception network or reproductive law specialist can help navigate these complex legal issues and ensure both partners’ interests are protected.
Understanding Sperm Donor Rights and Responsibilities
When using an anonymous sperm donor from a reputable sperm bank, the donor has no legal rights or responsibilities to any resulting children (in most U.S. states). However, if using a known donor, explicit legal agreements must be in place to clarify whether the donor will have any parental or financial involvement.
Some couples choose to use a known donor to maintain a connection or for cultural reasons. In these cases, working with a reproductive lawyer to create a clear donor agreement is essential.
Choosing Your Fertility Clinic and Sperm Bank
Selecting a Fertility Clinic
When choosing a fertility clinic, consider:
-
Expertise and experience with LGBTQ+ patients
-
Success rates (though remember these vary by patient age and clinic)
-
LGBTQ+ reviews and testimonials
-
Location and convenience
-
Costs and payment plan flexibility
-
Laboratory technology (does the clinic use AI Embryo Monitoring or other advanced techniques?)
-
Psychological support services
-
Relationship with reputable sperm banks
Leading clinics with strong LGBTQ+ programs include CNY Fertility, Pacific Fertility Center Los Angeles, and CCRM Fertility.
Selecting a Sperm Bank
When choosing a sperm bank and sperm donor:
-
Verify the bank is accredited and follows FDA regulations
-
Review the sperm donor health history and genetic screening
-
Decide between ID-release and non-ID-release donors (in UK and some other countries, only ID-release donors are permitted)
-
Consider whether you want donor information available to your child later
-
Understand costs and storage policies
-
Confirm shipping and handling procedures to maintain sperm sample viability
Reputable sperm banks screen donors for genetic disorders, infectious diseases, and provide detailed phenotypic information.
Conclusion
Reciprocal IVF offers a powerful and unique path to parenthood for LGBTQ+ families, allowing two individuals to share in the biological creation of their child. The journey involves a series of carefully planned medical steps, from ovarian stimulation and egg retrieval to embryo transfer. While the process is emotionally rewarding, it demands significant financial planning, with costs that encompass the base cycle, medications, donor sperm, and potential genetic testing.
Navigating the complexities of insurance coverage is a critical challenge, but growing advocacy and inclusive fertility benefits providers like Progyny, Carrot, and WINFertility are creating more accessible pathways. Success rates are promising—and improving year over year—yet they hinge on factors like the age of the egg provider and the expertise of the fertility clinic. Finally, securing legal parenthood for both partners through second-parent adoption is an essential step to protect your family.
By arming yourself with comprehensive information, seeking expert medical and legal guidance, and connecting with support communities through the LGBTQ+ community and donor conception network, you can confidently embark on this beautiful, shared journey to motherhood. The path to building your family through Reciprocal IVF is increasingly accessible, supported, and celebrated.
Key Resources:
-
American Society for Reproductive Medicine (ASRM): www.asrm.org
-
Centers for Disease Control and Prevention (CDC): Fertility/Infertility data
-
Society for Assisted Reproductive Technology (SART): Success rate calculator
-
RESOLVE: Insurance advocacy and resources
-
Family Equality: Grants and support for LGBTQ+ families