The Profound Decision of Embryo Transfer
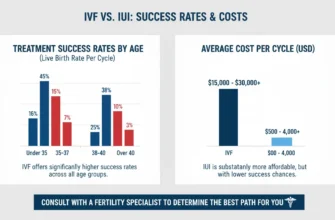
Navigating the world of reproductive medicine involves a series of deeply personal and complex decisions. Among the most pivotal is determining the number of embryos to transfer during an in vitro fertilization (IVF) cycle. For patients who have endured a long and emotional journey, the idea of transferring three embryos can seem like a way to maximize the chances of a successful pregnancy. However, this decision carries a significant increase in the likelihood of multiple pregnancies, including the high-stakes possibility of triplets. This article aims to demystify the odds, explore the influencing factors, and provide a clear, comprehensive understanding of what a 3 embryo transfer truly entails.
The Emotional Landscape of Fertility Treatments
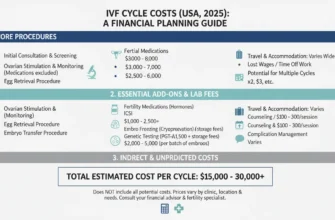
The path to building a family through IVF is often fraught with hope, anxiety, and substantial investment—emotionally, physically, and financially. Each cycle represents a new wave of possibility, and the desire for a live birth can be all-consuming. This emotional weight heavily influences decisions made alongside a fertility specialist, where the goal is to balance the highest chance of success with the lowest possible risk. Patient autonomy in this process is critical, requiring full informed consent about the realities of multiple embryo transfer decisions.
Understanding the Scope of a 3 Embryo Transfer
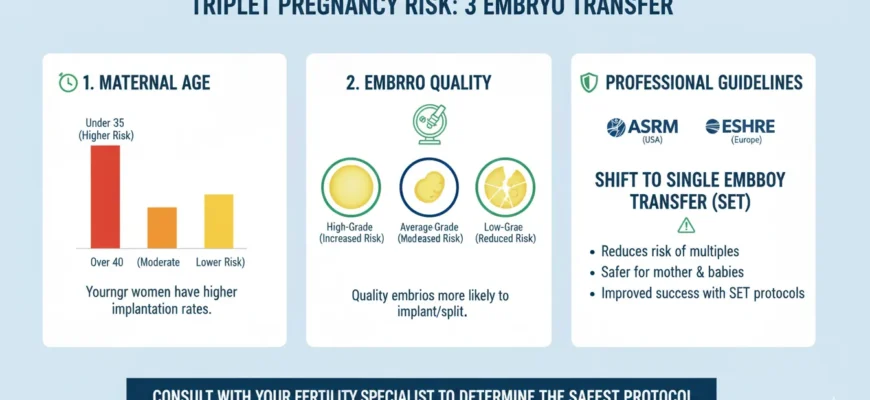
A 3 embryo transfer is a procedure where three embryos are placed into the uterus with the hope that at least one will achieve implantation. While this approach was more common in the past, advances in reproductive medicine and updated professional guidelines have shifted the focus decisively toward transferring fewer, higher-quality embryos. Today, a multiple embryo transfer of this number is rarely recommended and typically reserved for very specific clinical scenarios. Both the American Society for Reproductive Medicine (ASRM) and the European Society for Human Reproduction and Embryology (ESHRE) now strongly recommend against transferring more than two embryos in most clinical situations, with the goal of achieving singleton pregnancies while maintaining cumulative live birth rates across multiple cycles.
The Foundation: What is a 3 Embryo Transfer?
Understanding the context of a 3 embryo transfer requires a basic knowledge of the IVF process and the clinical reasoning that might lead to such a decision. It is a specific type of multiple embryo transfer designed to increase pregnancy rates in certain patient populations, though current evidence and guidelines indicate this strategy carries substantial risks that often outweigh potential benefits.
The IVF Process and Embryo Transfer
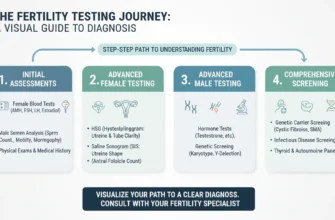
The IVF journey begins with ovarian stimulation, followed by egg retrieval and fertilization in a laboratory. The resulting embryos are cultured for several days, typically to the cleavage stage (Day 3) or the blastocyst stage (Day 5 or 6). The embryo transfer is the final, crucial step where one or more selected embryos are carefully placed into the patient’s uterus. The ultimate goal is for an embryo to implant into the uterine lining, leading to a successful pregnancy.
Rationale Behind Transferring Three Embryos
Historically, the primary reason a fertility specialist might consider transferring three embryos was to overcome a lower per-embryo implantation rate. The logic was that by transferring more embryos, the statistical probability that at least one would implant increases. This strategy was sometimes employed for patients over 37 years of age, those using embryos of lower quality, or individuals who had not become pregnant after previous transfer cycles with fewer embryos. However, current professional guidelines strongly advise against this approach due to the compounding risks of multiple birth.
Current ESHRE and ASRM guidance (2021, 2024) explicitly states that no clinical or embryological factor per se justifies a recommendation of transferring more than two embryos instead of a single embryo transfer (SET) in most circumstances. Transfer of more than two embryos is now considered non-standard practice in contemporary reproductive medicine.
The Biology of Multiples: How Triplets Can Arise from Three Embryos
When three embryos are transferred, a triplet pregnancy is a direct and foreseeable possibility. Understanding how this happens involves looking at the biological processes of implantation and embryo development.
The Implantation Process
Implantation is the delicate process where an embryo attaches to the wall of the uterus. For a triplet pregnancy to occur from a 3 embryo transfer, all three separate embryos must successfully implant and continue to develop. Each embryo’s success is an independent event, yet they are all influenced by the same key factors: the quality of each embryo and the receptivity of the uterine environment during that specific cycle. Endometrial receptivity—the ability of the uterine lining to accept and support an implanting embryo—is a critical factor. A successful implantation for all three results in fraternal (trizygotic) triplets.
Zygosity and Triplet Formation
The most straightforward way to get triplets from a 3 embryo transfer is for each of the three embryos to implant, resulting in trizygotic triplets, who are genetically distinct siblings. However, other, rarer possibilities exist. For instance, two embryos could implant, and one of those could split spontaneously (a phenomenon known as embryo splitting), resulting in a set of identical (monozygotic) twins and a singleton. Even more rarely, one embryo could implant and then split into three, forming identical monozygotic triplets, while the other two embryos fail to implant. Additionally, monozygotic twins can occur spontaneously after single embryo transfer in 0.9–2.2% of cases.
Deciphering the Odds: Key Factors Influencing Triplet Chances
The probability of a triplet pregnancy following a 3 embryo transfer is not a single, fixed number. It is a dynamic outcome influenced by a confluence of biological and clinical factors, each playing a critical role in the implantation rate of the embryos.
Embryo Quality and Stage: The Cornerstone of Success
Embryo quality is arguably the most important predictor of success. High-quality, euploid (chromosomally normal) embryos have a much higher implantation rate. Transferring three high-grade blastocysts carries a substantially higher risk of triplets than transferring three lower-grade, cleavage-stage embryos. Preimplantation genetic testing (PGT-A) can identify euploid embryos, which strengthens the case for a single embryo transfer to achieve a healthy live birth while avoiding multiple birth risks.
Research shows that women with three chromosomally-normal embryos have approximately a 95% cumulative chance of achieving pregnancy across consecutive single embryo transfers, with individual implantation rates of 69.4% for the first transfer, 59.3% for the second, and 59.2% for the third. This demonstrates that using consecutive single transfers of high-quality embryos achieves superior cumulative outcomes compared to transferring multiple embryos in a single cycle, with dramatically reduced risk of multiples.
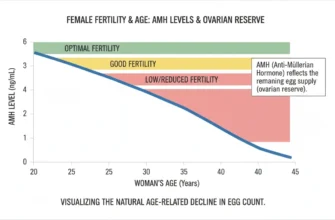
Maternal Age: A Significant Predictor
A patient’s age is intrinsically linked to egg and embryo quality. Younger patients (under 35) naturally have a higher likelihood of their embryos being chromosomally normal and, therefore, a higher implantation rate per embryo. Consequently, transferring three embryos in a younger patient dramatically increases the risk of a high-order multiple pregnancy. Current professional guidelines strongly recommend single embryo transfer for women under 38 years of age. For older patients, while the per-embryo chance of implantation is lower, this should not justify transferring more embryos; rather, it highlights the potential benefit of preimplantation genetic testing for aneuploidy to identify the healthiest available embryos for transfer.
The relationship between maternal age and embryo quality is profound: approximately 70% of embryos from women under 30 are euploid, compared to only 15% of embryos from women over 43.
Uterine Environment and Endometrial Receptivity
A successful pregnancy depends on more than just the embryo; the uterus must be ready to receive it. The thickness and quality of the endometrial lining are important factors for implantation. Factors like uterine fibroids, polyps, or other structural issues can hinder implantation rates, affecting the outcome of the transfer regardless of the number of embryos used. Body mass index (BMI) is another modifying factor; obesity is associated with decreased clinical pregnancy rates and increased miscarriage risk in both fresh and frozen embryo transfer cycles.
Previous Pregnancy History and IVF Outcomes
A patient’s reproductive history provides valuable data for a fertility specialist. A history of successful pregnancies may suggest a favorable uterine environment, potentially increasing the odds of multiple implantations. Conversely, multiple failed IVF cycles might suggest underlying implantation issues, which are better addressed through investigation and optimization rather than simply transferring more embryos.
Other Modifying Factors
Lifestyle factors such as smoking and obesity can negatively impact IVF outcomes and implantation rates. Additionally, the specific protocols used by the fertility center and the experience of the embryology lab can influence embryo quality and, by extension, pregnancy rates. The use of techniques such as assisted hatching can affect outcomes, though current evidence does not support using these as justifications for multiple embryo transfer. Hormonal support during the luteal phase (progesterone supplementation) and proper embryo culture conditions are also critical for optimizing implantation success.
Quantifying the Odds: Specific Triplet Probabilities with 3 Embryo Transfer
While patients understandably want precise numbers, calculating exact odds of triplets is complex. The probability is highly individualized, but we can explore illustrative ranges based on the key factors discussed.
The Complexity of Precise Statistics
It’s challenging to provide a single statistic because a 3 embryo transfer is no longer a common practice in many parts of the world, especially for younger patients with good-quality embryos. Clinical data is often stratified by age and embryo stage, and the outcome depends heavily on the individual implantation rate of each of the three embryos. Historical data from 2003-2006 provides some reference points: one study found triplet rates of 7.7% with 3 embryo transfers, though this varied significantly based on embryo quality.
Research from older datasets examining clinical decision-making found that when transferring 3 embryos, the predicted probability of multiple gestation ranged from approximately 2.7% to over 30%, depending heavily on maternal age and previous reproductive history. Among cycles ending in live birth from studies using historical data, 2.9% resulted in triplet births when multiple embryos were transferred.
Estimating Chances Based on Key Scenarios (Illustrative Ranges)
To illustrate the variability, consider these hypothetical scenarios:
Younger Patient (<35) with High-Quality Blastocysts: The individual implantation rate per embryo could be as high as 40-50%. In this case, the chance of a triplet pregnancy could be substantial, potentially in the 5-10% range or even higher, with the risk of twins being significantly greater. However, current guidelines explicitly recommend against this approach; instead, consecutive single embryo transfers would achieve the same or better cumulative outcomes with minimal risk of multiples.
Older Patient (>40) with Day 3 Embryos of Average Quality: The individual implantation rate per embryo might be much lower, perhaps 10-15%. Here, the primary goal is to achieve any pregnancy. The chance of triplets would be lower, likely in the 1-3% range, but the risk of twins would still be elevated compared to a single embryo transfer. Even in this scenario, current guidelines recommend single embryo transfer, potentially with selection of high-quality embryos through embryo grading or PGT-A testing.
These are not definitive predictions but demonstrate how the underlying variables dramatically alter the potential outcomes of the transfer.
The Impact of Vanishing Twin and Pregnancy Loss
It is important to remember that not all implantations result in a live birth. The rate of pregnancy loss is naturally higher in multiple pregnancies. An early ultrasound might show three gestational sacs, but one or more may not continue to develop—a phenomenon known as a “vanishing twin” or vanishing triplet. Research indicates that vanishing twin syndrome occurs in 5-30% of multiple pregnancies after IVF, with the fetal heartbeat visible on first-trimester ultrasound being a critical milestone. Therefore, the rate of triplet live births is typically significantly lower than the initial triplet implantation rate.
Studies show that survivors of a vanishing twin have adverse outcomes including lower birth weight, increased risk of prematurity, and potential neurological sequelae, especially if the vanishing occurs late in the first trimester. Among IVF singletons born, approximately 10% originated from twin gestations that resulted in a vanishing twin.
The Realities and Risks of Triplet Pregnancies
The goal of fertility treatment is a healthy baby and a healthy parent. A triplet pregnancy, while sometimes viewed as an instant family, carries profound risks that challenge this primary objective. The incidence of triplet and higher-order births in the United States has declined dramatically by 64% from 1998 to 2023, largely due to guideline implementation recommending fewer embryos transferred.
Maternal Health Complications
Mothers carrying triplets face a dramatically increased risk of serious health issues:
-
Preeclampsia (dangerously high blood pressure) with significantly elevated rates
-
Gestational diabetes with substantially higher incidence than singleton pregnancies
-
Severe anemia requiring management and possible transfusion
-
Antepartum hemorrhage and postpartum hemorrhage with increased severity
-
Cesarean delivery requirements
-
Pregnancy-induced hypertension
The physical strain on the body is immense, and the pregnancy is almost guaranteed to require intensive monitoring and specialized care. Women carrying triplets typically experience more frequent prenatal complications and higher rates of medical intervention.
Fetal and Neonatal Risks
The greatest risk for the babies is premature birth. The vast majority of triplet pregnancies deliver prematurely, often before 32 weeks, with a median gestational age around 32-34 weeks compared to 40 weeks for singletons and 36 weeks for twins. This leads to:
-
Low birth weight and very low birth weight (extremely common)
-
High likelihood of a prolonged stay in the Neonatal Intensive Care Unit (NICU)
-
Respiratory problems and potential need for ventilatory support
-
Retinopathy of prematurity
-
Necrotizing enterocolitis
-
Intraventricular hemorrhage
-
Cerebral palsy and developmental delays
-
Increased neonatal mortality
Over 50% of triplets are born with low birth weight (below 2,500 grams), and over 60% are born prematurely. These conditions are associated with significant long-term health challenges and increased risk of neurodevelopmental disabilities.
Practical, Emotional, and Financial Challenges
Beyond the medical risks, raising triplets presents enormous logistical, emotional, and financial challenges. The cost of care, the need for specialized equipment and support, and the sheer intensity of caring for three infants simultaneously can place immense strain on a family. Postpartum mental health challenges, including depression and anxiety, are more common in parents of multiples. The increased financial burden of hospital care for premature infants and ongoing specialized care for potential disabilities can create lasting economic stress.
Professional Guidelines and Current Recommendations
The Role of Professional Society Guidelines
Organizations like the American Society for Reproductive Medicine (ASRM) and the European Society for Human Reproduction and Embryology (ESHRE) provide guidelines to help clinics and patients make safe and effective decisions. The most recent guidance (ASRM 2021, ESHRE 2024) strongly advocates for minimizing the number of embryos transferred to reduce the rate of multiple pregnancies:
-
ASRM 2021 Guidance recommends single embryo transfer for women under 38 years of age with favorable prognosis, and explicitly states that for patients 38-40 years old with untested embryos, no more than 3 cleavage-stage or 2 blastocysts should be transferred.
-
ESHRE 2024 Guideline provides an even stronger recommendation: “No clinical or embryological factor per se justifies a recommendation of double embryo transfer instead of single embryo transfer,” and explicitly recommends against the transfer of more than two embryos with fetal reduction after multiple implantation, considering the high risks.
For most favorable patient profiles, single embryo transfer (SET) is now recommended as the gold standard approach. The guideline development process reviewed over 17,700 scientific articles and found strong evidence supporting this approach.
The Fertility Specialist’s Crucial Role
Your fertility specialist is your most important partner in this process. They will use their expertise to evaluate all your individual factors—age, embryo quality, past cycles, endometrial receptivity, and overall health—to provide a personalized recommendation. Their role is to help you understand the realistic pregnancy rates for your specific situation and to clearly outline the risks associated with a multiple embryo transfer. They should document any justification for transferring more embryos than recommended, as required by professional guidelines.
Patient Autonomy and Informed Consent
Ultimately, the decision is yours. True informed consent means you have a complete and unvarnished understanding of all potential outcomes—not just the chance of pregnancy, but the specific, quantifiable risks of a twin or triplet pregnancy. It is about making a choice that aligns with your hopes and your capacity to handle the potential challenges. However, professional guidelines emphasize that patients should be fully informed of the medical evidence supporting single embryo transfer, and that financial considerations (cost of additional cycles) should not be the driving factor in this decision.
Strategies for Optimizing Outcomes and Mitigating Risks
Modern reproductive medicine has evolved to focus on a new definition of success: the healthy singleton birth. This approach has proven to maximize long-term family outcomes while reducing maternal and fetal risks.
The Gold Standard: Single Embryo Transfer (SET)
For many patients, especially those with high-quality blastocysts identified through methods like preimplantation genetic testing, transferring a single embryo offers a comparable or superior chance of a successful pregnancy compared to transferring multiple embryos, but without the associated risks. The goal of single-embryo transfer is to mimic natural conception, leading to a safer pregnancy and healthier outcome for both mother and child. When a cycle produces multiple high-quality embryos, the remaining ones can be frozen embryos for future attempts, offering more opportunities for a family without the risks of a multiple birth.
Research demonstrates that women with three euploid embryos achieve approximately a 95% cumulative pregnancy rate across three consecutive single embryo transfers, demonstrating that this approach is both safe and highly effective. This strategy aligns with the recommendations from both ASRM and ESHRE.
Preimplantation Genetic Testing (PGT-A)
Preimplantation genetic testing for aneuploidy (PGT-A) has transformed the field by allowing selection of chromosomally-normal embryos. This technology enables higher implantation rates with single embryo transfer compared to untested embryos, particularly for older patients. Approximately 50% of embryos are euploid on average, with higher rates in younger women and lower rates in older women. The use of PGT-A can identify those embryos most likely to result in pregnancy, reducing the need for multiple embryo transfer in most scenarios.
Frozen Embryo Transfer and Cumulative Success
Frozen embryo transfer (FET) has become increasingly important in optimizing outcomes. Modern vitrification techniques have improved significantly, with survival rates of frozen embryos now approaching 95%. By using consecutive frozen embryo transfers of single, high-quality embryos (especially euploid blastocysts), couples can achieve excellent cumulative live birth rates while maintaining the safety profile of singleton pregnancies.
Conclusion
The decision to transfer three embryos in a single IVF cycle is now recognized as a non-standard approach that carries substantial risks without proportionate benefits. Current professional guidelines from both ASRM and ESHRE emphasize that single embryo transfer represents the optimal strategy for most patients, with rare exceptions that require careful documentation and justification.
While the emotional desire to maximize pregnancy chances in a single cycle is understandable, the evidence overwhelmingly supports a strategy that prioritizes maternal and fetal health through more conservative embryo transfer practices combined with the opportunity for multiple cycles using frozen embryos. This approach not only reduces the risk of life-threatening maternal complications and serious neonatal morbidity, but also achieves superior cumulative success rates across multiple transfer attempts.
Patients considering IVF should have detailed conversations with their fertility specialist about personalized strategies that balance their individual prognosis with the well-established medical evidence supporting single embryo transfer. In most cases, this represents the safest and most effective path to building a healthy family.