Unlocking Insights into Your Ovarian Reserve
Navigating the path to parenthood or simply seeking to understand your reproductive health can feel overwhelming. With a vast amount of information available, it’s easy to get lost in complex medical terminology. One of the most powerful tools available for insight into female fertility is the Anti-Müllerian Hormone (AMH) blood test. This simple test provides a crucial snapshot of your ovarian reserve, offering valuable data that can inform your family planning decisions and help you understand your reproductive timeline.
What is AMH and Why is it Important for Fertility?
Anti-Müllerian Hormone, or AMH, is a protein hormone produced by the small, developing follicles within the ovaries. The level of this hormone in your bloodstream correlates directly with the number of eggs you have remaining. As a result, an AMH blood test is one of the most reliable indicators of your ovarian reserve—a term used to describe the quantity of your remaining egg supply. Understanding your AMH level is a critical first step in any comprehensive fertility assessment.
The name “anti-Müllerian” comes from AMH’s developmental role: in male embryos, it causes the regression of the Müllerian ducts (also called paramesonephric ducts), which would otherwise develop into the uterus and fallopian tubes. This hormone is essential for proper male sexual differentiation during fetal development. In adult females, AMH takes on a different role, serving as an important marker of ovarian function and the aging of the egg supply.
The Purpose of This Guide: Demystifying Your Reproductive Health Journey
This guide is designed to demystify the AMH Blood Test. We will explore what AMH is, how the test works, what your results mean, and most importantly, what your next steps should be. Whether you are actively trying to conceive, considering fertility treatment, or simply planning for the future, this information will empower you to have more informed conversations with your healthcare provider and take control of your reproductive health journey.
What is Anti-Müllerian Hormone (AMH)?
To fully grasp the significance of the AMH test, it’s essential to understand the hormone itself and its fundamental role in ovarian function. AMH is a key player in the development of reproductive organs and serves as a direct biological marker of your egg count throughout your reproductive years.
The Role of AMH in Ovarian Function and Follicle Development
AMH is produced by granulosa cells, which are found in the small, preantral and early antral ovarian follicles. These are the developing follicles that house immature eggs. The hormone plays a regulatory role, helping to control the development of these follicles. In essence, it ensures that only a select number of follicles of the ovaries are recruited to grow and mature each month, preventing premature depletion of the entire egg supply. This makes its level a direct reflection of the underlying follicular activity in the ovaries.
How Granulosa Cells Produce AMH
Every month, a group of tiny follicles is activated from the dormant pool, beginning the process of folliculogenesis. The granulosa cells surrounding the eggs within these developing small follicles begin to produce AMH. The more developing follicles there are, the more AMH is released into the bloodstream. As a woman ages and the number of available follicles naturally declines, the production of AMH decreases in parallel. This direct relationship is what makes the hormone testing through AMH measurement such a valuable tool for measuring ovarian reserve.
AMH’s Connection to Ovarian Reserve and Egg Count
Ovarian reserve refers to the quantity of eggs remaining in the ovaries. A higher AMH level generally indicates a larger pool of remaining primordial follicles and growing follicles, and by extension, a higher egg count. Conversely, a lower AMH level suggests a diminished ovarian reserve (DOR). It is crucial to remember that AMH reflects egg quantity, not quality. Egg quality is primarily determined by age and is a separate, though equally important, factor in overall fertility.
The AMH gene on chromosome 19p13.3 encodes this hormone, while its receptor (AMHR2) is encoded on chromosome 12. Understanding the genetic basis of AMH production helps clarify why variations exist between individuals in their hormone levels and ovarian responses to stimulation.
Understanding the AMH Blood Test
The AMH blood test is a straightforward procedure that provides significant insights. It is a cornerstone of modern fertility workups, offering a clear, data-driven look at one aspect of your reproductive potential.
Why Your Doctor Might Recommend an AMH Test
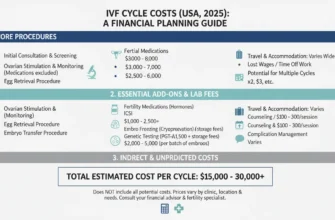
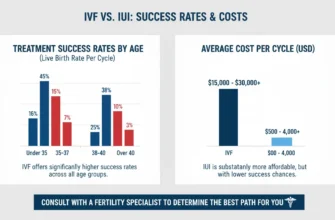
A doctor or fertility specialist may recommend an AMH test for several reasons. It is a standard part of a fertility assessment for individuals or couples struggling to conceive. It is also used to help predict how well a woman might respond to ovarian stimulation during fertility treatment like in vitro fertilization (IVF). Furthermore, it can be a proactive measure for those who want to understand their reproductive timeline for family planning or are considering egg freezing. The test is also used in the evaluation of conditions like polycystic ovary syndrome (PCOS) and to help predict the onset of menopause. Additionally, AMH testing is valuable for cancer survivors who have undergone gonadotoxic therapy or chemotherapy, as it helps assess reproductive lifespan and remaining fertility options.
The AMH Blood Test Procedure: What to Expect During a Blood Draw
The AMH blood test is a simple blood test. A healthcare professional will collect a small blood sample from a vein in your arm, typically at the elbow. The procedure is quick, usually taking less than five minutes, and involves minimal discomfort. The collected blood sample is then sent to a laboratory for analysis.
Preparing for Your AMH Test: Are Cycle Days Important?
One of the significant advantages of the AMH test compared to other hormone tests is its stability. AMH levels do not fluctuate significantly throughout the menstrual cycle. This means the blood draw can be taken on any day of your cycle, offering convenience and flexibility in scheduling. No special preparation, such as fasting, is required. While some sources recommend testing between days 5 and 10 of the menstrual cycle for optimal consistency, this is not a strict requirement due to AMH’s cycle-independent nature. This flexibility is one reason AMH has become more popular than older tests requiring specific cycle days for measurement.
How AMH Levels Are Measured and Reported
Labs measure the concentration of AMH in your blood. Results are typically reported in nanograms per milliliter (ng/mL) or picomoles per liter (pmol/L). It’s important to pay attention to the units used by your specific lab, as the numerical values will differ—approximately 1 ng/mL equals 7 pmol/L. Your report will show your serum antimüllerian hormone levels, often alongside a reference range for your age group, allowing for a direct comparison.
Interpreting Your AMH Levels: What the Numbers Mean
Receiving your AMH results is a pivotal moment, but the numbers require careful interpretation. Your level should always be considered within the context of your age and overall health, and discussed with a qualified professional.
General AMH Level Ranges by Age
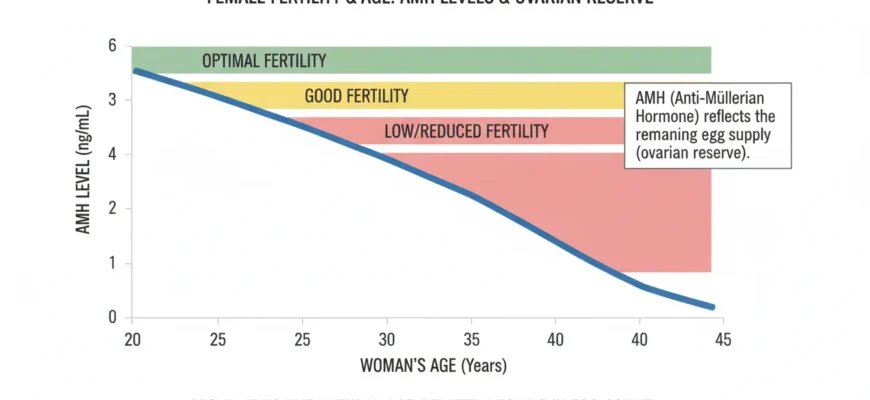
AMH levels are highest during a woman’s mid-twenties and gradually decline with age. Research shows that AMH peaks around age 24.5 years, after which it steadily decreases until menopause. While specific ranges can vary by laboratory and testing method used, general guidelines are:
For women under 25: 3.0 to 5.0 ng/mL is often considered optimal.
For women 25-30: 2.5 to 4.0 ng/mL may be typical.
For women 30-35: 1.5 to 3.5 ng/mL is generally expected.
For women 35-40: 1.0 to 3.0 ng/mL represents typical ranges.
For women 40-45: 0.5 to 2.0 ng/mL is common.
For women over 45: Below 1.0 ng/mL is typical, with levels often below 0.5 ng/mL.
Very low levels (e.g., <0.5 ng/mL) suggest a significantly diminished ovarian reserve. These are general estimates, and a fertility specialist will interpret your specific number based on your individual profile, age, and other diagnostic markers.
What Low AMH Levels Can Indicate: Diminished Ovarian Reserve and Reproductive Lifespan
A low AMH level for your age indicates diminished ovarian reserve (DOR), meaning you have fewer remaining eggs than is typical for your age group. This can suggest a shorter reproductive lifespan and may mean that the window for conception is narrowing. It can also predict a lower response to ovarian stimulation for treatments like IVF, potentially resulting in fewer eggs retrieved. However, it’s important to note that low AMH does not guarantee infertility—many women with low AMH still conceive naturally or successfully with assisted reproduction.
An AMH level below 0.61 ng/mL in serum is often associated with poor ovarian response during IVF protocols, though individual responses vary considerably. Some research suggests that an AMH cutoff of 0.5-1.1 ng/mL may identify women at risk for poor response, but these thresholds vary by laboratory and assay method.
What High AMH Levels Can Suggest: A Common Marker for Polycystic Ovary Syndrome (PCOS)
Conversely, a very high AMH level (often >4.0 ng/mL) can be a marker for Polycystic Ovary Syndrome (PCOS), a common hormonal imbalance affecting reproductive health. Women with polycystic ovaries (PCOS) tend to have a large number of small ovarian follicles, each producing AMH, which leads to an elevated overall level. While a high number might seem positive, in PCOS, these follicles often do not mature properly due to hormonal dysregulation, which can interfere with ovulation and fertility. PCOS is one of the most common reproductive health conditions, affecting 4-8% of women worldwide.
An AMH level above 3.9 ng/mL in serum may indicate PCOS, though age-specific thresholds improve diagnostic accuracy. It’s important to note that elevated AMH alone does not diagnose PCOS; the diagnosis requires meeting other criteria established by organizations like the Rotterdam Consensus.
The Nuance of AMH: Why It’s One Piece of the Fertility Puzzle
It cannot be overstated that AMH is just one piece of the puzzle. It is a powerful indicator of egg quantity but reveals nothing about egg quality, which is paramount for creating healthy embryos. A person with low AMH can still conceive with a high-quality egg, while someone with high AMH may struggle if egg quality is poor. Therefore, the AMH result must be integrated with other diagnostic information.
Important limitations of AMH include:
-
AMH does not predict egg quality: Egg quality is primarily age-dependent and cannot be determined by an AMH test.
-
AMH does not guarantee pregnancy: Many factors influence fertility beyond quantity of eggs, including sperm health, uterine health, reproductive tissues integrity, and hormonal imbalances.
-
AMH does not predict natural conception: While it predicts response to stimulation, it does not reliably predict the timing or likelihood of natural pregnancy.
-
Variability between cycles: AMH can fluctuate slightly between menstrual cycles, particularly in poor responders, though these variations are usually modest.
-
Assay differences: Different laboratory tests and assay methods can produce different results, which is why interpretation requires understanding your specific lab’s reference ranges.
Complementary Fertility Assessments: AFC Scan (Antral Follicle Count) and Other Hormone Tests
For a complete picture of your ovarian function, a fertility specialist will combine your AMH result with other tests. An Antral Follicle Count (AFC), performed via transvaginal ultrasound, visually counts the number of developing follicles in the ovaries. The AFC and AMH results usually correlate well and together provide a robust assessment of ovarian reserve. The correlation between AMH and ultrasound-visualized antral follicle count is strong, making these complementary markers valuable for fertility evaluation.
Other hormone tests, such as FSH (Follicle-Stimulating Hormone) and estradiol, are also used to evaluate the overall reproductive health landscape. FSH is typically measured on cycle days 2-3 when it is at baseline levels. Additionally, some fertility centers may recommend a Clomid Challenge Test (CCT) or other assessments to further characterize ovarian response patterns, though AMH has largely replaced these older tests due to its stability and reliability.
For women considering egg retrieval, the egg retrieval procedure itself will provide direct information about how many eggs can be obtained, which serves as the ultimate assessment of ovarian response to stimulation.
AMH and Your Fertility Journey: Planning for Conception
Your AMH level provides actionable insights that can directly influence your approach to family planning, whether you are trying to conceive naturally or exploring assisted reproductive technologies.
How AMH Levels Influence Natural Conception Prospects
While a low AMH level does not mean natural conception is impossible, it may indicate a need for greater urgency. Because it suggests a lower egg count, the time available for conception may be shorter. Research using time-to-pregnancy (TTP) studies has found that while there is a trend toward reduced fecundability in women with low AMH, the relationship is nuanced—optimal fertility occurs within a range of values, not simply above a single cutoff. Conversely, a normal AMH for your age provides some reassurance about your egg supply, though it doesn’t guarantee a successful pregnancy. It’s a measure of potential, not a definitive prediction of outcome.
AMH and Fertility Treatment: Guiding Your Options and IVF Protocols
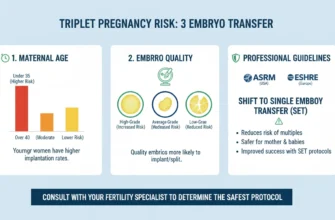
In the context of fertility treatment, AMH is a critical predictive tool. It helps a fertility specialist determine the appropriate type and dosage of medication for ovarian stimulation in treatments like in vitro fertilization (IVF). A higher AMH level may predict a robust response, yielding many eggs, while a lower AMH might lead to a more conservative protocol to maximize the yield from a smaller reserve.
IVF protocols are individualized based partly on AMH levels:
-
High responders (AMH >3.5 ng/mL) may require lower gonadotropin doses to avoid excessive ovarian response and ovarian hyperstimulation syndrome (OHSS).
-
Normal responders (AMH 1.5-3.5 ng/mL) typically use standard doses of stimulation medications.
-
Poor responders (AMH <1.0 ng/mL) may require higher gonadotropin doses or use of minimal stimulation protocols.
The Clomid Challenge Test, if performed, may also help refine stimulation protocols, particularly in older women or those with borderline AMH levels.
AMH as a Predictor: What It Can and Cannot Tell You
AMH Can Predict:
-
Your remaining egg count (ovarian reserve)
-
Your potential response to IVF protocols and ovarian stimulation medications
-
The approximate timing of menopause
-
Risk of ovarian hyperstimulation syndrome (OHSS) in high responders
-
Your menopausal status and transition to menopause
-
Gonadotoxic effects of chemotherapy and cancer treatment on ovarian reserve
AMH Cannot Predict:
-
The quality of your eggs
-
Whether you will Get Tested and achieve pregnancy in any given month
-
The exact timing of a successful conception
-
Your ability to conceive without assisted reproduction
-
Embryo quality or chromosomal normality
-
Whether you will experience pregnancy loss
Special Considerations: AMH in Specific Populations
Cancer Survivors and Gonadotoxic Therapy
For cancer survivors who have undergone chemotherapy or other gonadotoxic therapy, AMH testing is particularly valuable. Chemotherapy can cause rapid decline in blood levels of AMH and may damage or deplete the primordial follicle pool. Hormone therapy following cancer treatment may also suppress AMH levels.
Research demonstrates that:
-
High gonadotoxicity treatments (including high-dose alkylating agents and pelvic radiation) cause steep declines in AMH
-
Moderate and low gonadotoxicity treatments show more gradual decline and potential recovery
-
Age at treatment affects recovery: younger patients may show better AMH recovery than those treated after age 30
-
An undetectable AMH at end of cancer treatment has high sensitivity and specificity for predicting permanent premature ovarian insufficiency (POI) at 2 years post-treatment
For cancer survivors, AMH testing can help guide discussions about fertility preservation options like egg freezing or embryo freezing before treatment begins, or assess remaining options afterward.
Disorders of Sex Development
AMH testing is also used in the evaluation of ambiguous genitalia and other disorders of sex development (DSD). In individuals with undescended testicles (cryptorchidism) or persistent Müllerian duct syndrome, AMH levels can help distinguish between different types of sex development disorders by confirming the presence of functional testicular tissue.
Conditions Affecting Reproductive Health
Several reproductive health conditions and reproductive disorders can affect AMH levels:
-
Polycystic ovary syndrome (PCOS): Elevated AMH
-
Endometriosis: May be associated with slightly reduced AMH
-
Ovarian cancer or ovarian mass: May affect surrounding tissue and AMH production
-
Granulosa cell tumor: Can produce AMH and cause elevated levels
-
Pelvic scarring: From endometriosis, surgery, or other causes may reduce functional ovarian reserve
-
Thyroid disease: Autoimmune thyroid conditions may be associated with altered AMH levels
Navigating Your Next Steps: From Results to Action
Receiving your AMH result is not the end of the journey; it’s the beginning of an informed, proactive phase. Your next steps should be guided by professional advice tailored to your unique situation.
Consulting a Fertility Specialist: Why Expert Guidance is Crucial
Regardless of your AMH level, the most important next step is to discuss your results with a fertility specialist. They can interpret the number in the context of your age, medical history, other diagnostic tests, and reproductive goals. This expert consultation is crucial for avoiding misinterpretation and for creating a sound, evidence-based plan.
Specialized fertility centers like V Fertility Center and CREATE Fertility offer comprehensive evaluation and personalized treatment protocols based on individual AMH levels and other markers of ovarian reserve.
Your Comprehensive Fertility Assessment: Beyond the AMH Number
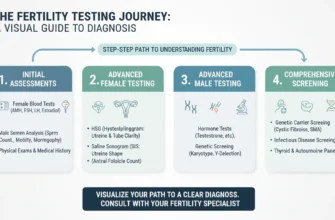
Your specialist will likely recommend a comprehensive fertility assessment. This goes beyond the AMH test to include:
-
AFC Scan (Antral Follicle Count) via transvaginal ultrasound
-
Other hormone tests (FSH, LH, estradiol)
-
Evaluation of your partner’s fertility, if applicable
-
Chromosome testing if indicated by history or results
-
Assessment of external sex organs and internal reproductive anatomy
-
Evaluation of potential reproductive tissues abnormalities
-
Screening for conditions like endometriosis or pelvic scarring
This holistic view is necessary to identify all factors that could be influencing your ability to conceive.
Developing a Personalized Family Planning Strategy
Armed with a complete assessment, you and your specialist can develop a personalized strategy. For someone with low AMH, this might involve:
-
Moving more quickly towards fertility treatment or assisted reproduction cycles
-
Considering options like egg freezing or embryo freezing to preserve fertility
-
Using ovarian stimulation protocols optimized for poor responders
-
Exploring ovarian rejuvenation options (though evidence remains limited)
For someone with high AMH indicative of PCOS, the plan may focus on managing ovulation and may include the Clomid Challenge Test or other ovulation induction strategies.
Exploring Lifestyle and Supportive Measures
While you cannot significantly increase your blood levels of AMH (as it’s tied to your finite egg supply), you can optimize your overall reproductive health. Maintaining a healthy weight, eating a balanced diet, avoiding smoking, and managing stress are all beneficial for ovarian function and can support egg retrieval outcomes and cycle outcome success in assisted reproduction. Regular exercise, adequate sleep, and supplementation (particularly CoQ10, vitamin D, and DHEA in some cases) may support fertility.
Exploring Advanced Options: Ovarian Rejuvenation
Ovarian rejuvenation using platelet-rich plasma (PRP) is an emerging, experimental treatment for women with low AMH and diminished ovarian reserve. While clinical evidence is still developing and results are mixed, some small studies have reported:
-
Increases in hormone levels including AMH
-
Improvements in antral follicle count
-
Increases in retrieved oocytes
-
Some reports of pregnancy even in women with very low AMH
However, ovarian rejuvenation remains experimental, and effectiveness has not been conclusively demonstrated in large, randomized controlled trials. Women considering this option should discuss realistic expectations with their fertility specialist.
The Importance of Fertility Counseling and Emotional Well-being
A fertility journey can be emotionally taxing. Seeking support from a counselor who specializes in fertility counseling and reproductive health can provide invaluable tools for managing stress and navigating the emotional highs and lows. Your mental well-being is a critical component of your overall health and can affect treatment outcomes. Assisted reproduction cycles and fertility treatment often involve significant emotional investment, and professional fertility counseling support is an important part of comprehensive care.
Special Considerations and Broader Reproductive Health
The AMH Blood Test is more than just a fertility marker; it’s a window into your broader reproductive health. It empowers you with knowledge about your body, allowing you to make proactive decisions about your future, whether that includes children or simply understanding your transition towards menopausal status and menopause.
Understanding hormone levels and your menopausal status earlier allows for informed family planning and family building decisions. By viewing the AMH test as one part of a larger wellness strategy, you can Get Tested, take control of your health journey with confidence and clarity, and make decisions aligned with your life goals.
Conclusion
The AMH blood test represents a significant advancement in understanding and managing fertility. As a marker of ovarian reserve, it provides valuable information about egg retrieval potential and ovarian response to stimulation. However, it is essential to remember that AMH is one component of a comprehensive fertility assessment and should be interpreted alongside other clinical markers, your age, chromosome testing results when indicated, and your personal reproductive goals.
Whether your AMH is high, low, or normal for your age, this knowledge empowers you to engage actively in your reproductive health decisions, work collaboratively with your fertility specialist, and pursue a path to parenthood or family planning that aligns with your values and circumstances. Modern fertility science, combined with comprehensive evaluation including transvaginal ultrasound and other hormone testing, offers hope and evidence-based treatment options for individuals at every stage of their fertility journey.
Key Takeaways
-
AMH measures ovarian quantity, not quality: It indicates how many eggs remain, not their genetic health or viability
-
Age-appropriate interpretation is critical: The same AMH number means different things at different ages
-
AMH guides, but doesn’t determine, fertility outcomes: Many factors beyond AMH influence conception success
-
Comprehensive evaluation is essential: Combine AMH with AFC, FSH, age, and other markers for complete picture
-
Professional guidance ensures accurate interpretation: Always discuss results with a fertility specialist
-
Early testing can inform family planning: Understanding your AMH helps with proactive decision-making about fertility preservation and family building timeline