Navigating Your Fertility Journey with Lab Tests
Navigating the path to parenthood can be a complex and emotional journey, and when conception doesn’t happen as expected, uncertainty can be overwhelming. Fortunately, modern medicine offers a clear roadmap to understanding your reproductive health: fertility lab tests. These diagnostic tools are the first and most crucial step in identifying potential obstacles and creating a personalized plan to achieve your family-building goals. This guide provides a comprehensive overview of the essential blood tests for both men and women, demystifies at-home fertility tests, and explains what your results truly mean, empowering you with the knowledge needed to take control of your fertility journey.
Who Should Consider Fertility Testing?
Fertility testing is generally recommended for couples who have been trying to conceive without success. The standard guideline is to seek an evaluation after one year of regular, unprotected intercourse if the female partner is under 35, or after six months if she is 35 or older. Individuals with known risk factors, such as a history of pelvic inflammatory disease, irregular menstrual cycles, previous cancer treatment, or a known male factor issue, should consider consulting a specialist sooner. Testing is also vital for those planning for fertility preservation and individuals with conditions like premature ovarian insufficiency.
The Role of Lab Tests in Understanding Infertility
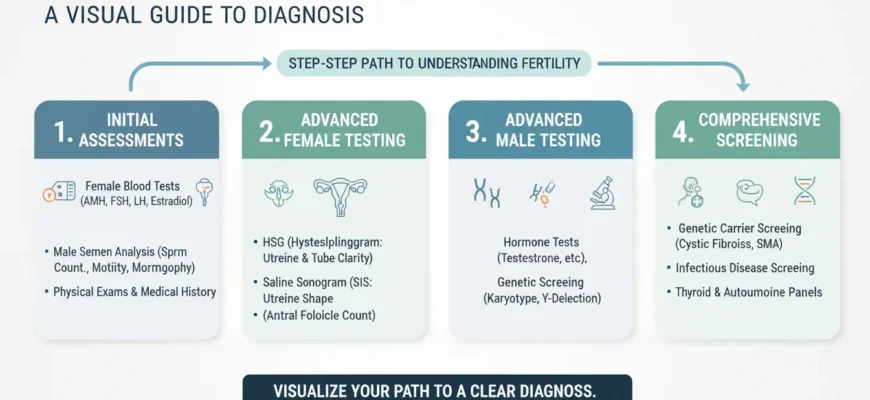
Lab tests serve as the foundation of a fertility evaluation. They provide objective data that helps fertility specialists pinpoint the underlying causes of infertility, which can stem from hormonal imbalances, issues with egg or sperm production, or structural problems within the reproductive organs. By analyzing blood tests, semen, and imaging results, doctors can move from speculation to a clear diagnosis. This diagnostic clarity is essential for determining the most effective course of action, preventing wasted time on ineffective strategies.
Why Early and Comprehensive Testing Matters
Time is a critical factor in fertility. Early testing allows for prompt diagnosis and intervention, which can significantly improve the chances of a successful pregnancy. A comprehensive approach that evaluates both partners simultaneously is equally important. Infertility is a couple’s issue, with contributing factors found in men and women in roughly equal measure. By testing both partners from the outset, a complete picture of their combined fertility potential emerges, leading to a more targeted and effective fertility treatment plan.
Female Fertility Testing: Uncovering Reproductive Potential
For women, fertility testing focuses on three primary areas: ovarian reserve (the supply of eggs), hormonal function and ovulation, and the physical health of the reproductive organs. A combination of blood tests and imaging provides a detailed assessment of these key components.
Ovarian Reserve Testing: Assessing Your Egg Supply
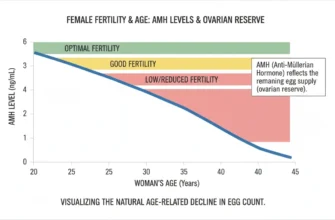
Ovarian reserve refers to the quantity and quality of a woman’s remaining eggs. As a woman ages, this supply naturally declines. Several tests are used to estimate this reserve:
Anti-Müllerian Hormone (AMH): This blood test measures a hormone produced by developing follicles in the ovaries. AMH Levels are a stable indicator of the remaining egg supply. A higher level generally suggests a larger reserve, while a very low level may indicate diminished ovarian reserve. Normal AMH test results typically range from 1.0–3.5 ng/mL for optimal response to fertility treatment, though normal values can vary. AMH testing should be assessed approximately once every three months for tracking purposes.
Follicle-Stimulating Hormone (FSH): Follicle-stimulating hormone is a hormone that stimulates the growth of follicles in the ovaries each month. This blood test, typically done on day 3 of the menstrual cycle (cycle day 2-3 FSH), reveals how hard the body is working to produce an egg. Elevated FSH Levels can suggest a declining ovarian reserve, though FSH Levels should be interpreted alongside other markers.
Estradiol: Tested alongside FSH, this hormone helps interpret FSH results. High early-cycle estradiol can artificially suppress FSH, masking potential issues.
Antral Follicle Count (AFC): A Transvaginal Ultrasound (also called pelvic ultrasound) is used to count the number of small, visible follicles in the ovaries at the beginning of the menstrual cycle. This count provides a real-time visual assessment of the potential eggs available for recruitment. Normal antral follicles typically range from 3-30 total, with 12-24 being common, though this varies significantly by age.
Ovulation & Hormonal Function Tests
Confirming that ovulation—the release of an egg from the ovary—is occurring regularly is fundamental to fertility. Several Hormone Levels are checked via blood tests to evaluate this process:
Luteinizing Hormone (LH): A surge in Luteinizing Hormone triggers ovulation. While often tracked with at-home fertility tests and Home Urine LH Testing, a LH blood test can confirm LH levels and help time fertility treatments. An ovulation predictor kit can also detect this surge in urine.
Progesterone: This hormone rises after ovulation to prepare the uterine lining for a potential pregnancy. A blood test performed approximately 7 days after ovulation (often called “day 21” testing in a 28-day cycle) can confirm whether an egg was successfully released. A progesterone level above 5 ng/mL confirms ovulation occurred, with ideal levels at 10 ng/mL or higher.
Other Hormones: Thyroid-stimulating hormone (TSH) and prolactin are also routinely checked. Imbalances in these hormones can disrupt the menstrual cycle and interfere with Ovulatory Function. Female fertility blood test results should always be interpreted alongside clinical history and other test results.
Assessing Uterine & Fallopian Tube Health
Beyond hormones and eggs, the physical structures of the reproductive system must be healthy. A Transvaginal Ultrasound is a key diagnostic tool that allows fertility specialists to examine the uterus for abnormalities like fibroids or polyps and to visualize the ovaries.
For the fallopian tubes, a procedure called a hysterosalpingogram (HSG) may be recommended to ensure they are open and free of blockages that could prevent the egg and sperm from meeting. The HSG procedure uses contrast dye injected into the uterine cavity to visualize the uterus and fallopian tubes, identifying any structural abnormalities or scarring inside the uterus lining. If abnormalities are suspected, a saline sonogram (sonohysterography) may be performed as an alternative or supplementary ultrasound technique.
Male Fertility Testing: Understanding Sperm Health and Function
Male factor infertility contributes to nearly half of all infertility cases, making a thorough evaluation of the male partner essential. Testing primarily focuses on the production and function of sperm.
Semen Analysis: The Foundational Test
The cornerstone of male fertility testing is the semen analysis. This non-invasive test provides a comprehensive assessment of sperm health by examining a sample of semen. Key parameters measured include:
Sperm Count (Concentration): The number of sperm per milliliter of semen. According to the WHO 2021 sixth edition criteria, a low sperm count (oligozoospermia) is defined as fewer than 15 million sperm per milliliter. A low sperm count can reduce the chances of fertilization. The sample collection process requires 2-7 days of ejaculatory abstinence for standardization.
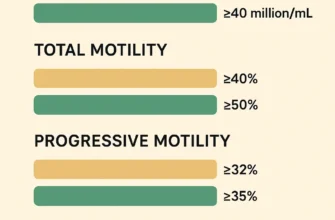
Motility: The percentage of sperm that are actively moving. According to WHO 2021 criteria, poor motility (asthenozoospermia) is defined as less than 40% total motility or less than 30% progressive motility. Healthy sperm must be able to swim effectively to reach and fertilize an egg. Sperm motility is a critical parameter for fertility potential.
Morphology (Shape): The percentage of sperm with a normal shape. Abnormal sperm morphology (teratozoospermia) means a high percentage of sperm have abnormal shapes and may have difficulty penetrating an egg. The WHO 2021 update changed some morphology assessment criteria compared to the 2010 edition.
Semen Volume: The total amount of ejaculate, typically 1.4 mL or greater per WHO 2021 standards. Low volume may indicate a blockage or other issue.
Post-ejaculatory urinalysis may be performed in cases where semen volume is low to rule out retrograde ejaculation.
Advanced Male Fertility Tests
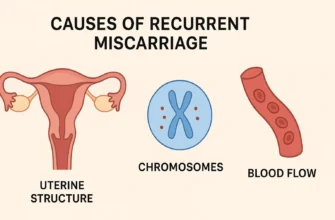
If a basic semen analysis shows abnormalities, or if infertility remains unexplained, further tests may be ordered. These can include Hormone Evaluation with testosterone, FSH, and LH levels, which are crucial for sperm production. In some cases, Genetic testing may identify chromosomal abnormalities through Karyotyping services or chromosome analysis, or a testicular biopsy might be performed to check for structural problems or retrieve sperm directly. Sperm DNA fragmentation testing may also be considered, particularly in cases of recurrent pregnancy loss, failed ART cycles, or men with high-risk lifestyle exposures, as it can provide additional diagnostic information beyond conventional parameters. Additionally, advanced tests may assess response to fertility medication or evaluate sperm function at the molecular level.
Integrated & Advanced Fertility Testing for Both Partners
Sometimes, initial tests don’t reveal a clear cause for infertility. In these instances, more advanced and integrated testing can provide deeper insights by examining genetic and immunological factors.
Genetic Testing: Uncovering Heritable Factors
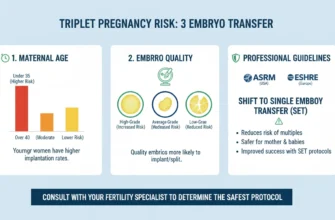
Genetic testing can be invaluable when there is a history of recurrent pregnancy loss, severe male factor infertility, or a family history of genetic disorders. Karyotyping services involve a blood draw that analyzes chromosome analysis for abnormalities that could affect fertility. Genetic carrier screening can determine if either partner carries a recessive gene for a specific condition that could be passed on to a child. This becomes particularly important for those considering assisted reproductive technology procedures like IVF with preimplantation genetic testing (PGT) to select unaffected embryos.
Immunological Testing (Brief Overview)
In some cases, the immune system may mistakenly attack sperm, an embryo, or reproductive tissues, leading to infertility or pregnancy loss. While complex and not routinely performed, immunological testing may be considered for individuals with unexplained infertility or recurrent implantation failure during fertility treatment like IVF. These tests look for specific antibodies or immune cell dysfunctions. However, standardized protocols and validated clinical indications remain an area of ongoing research.
Connecting the Dots: How Different Tests Create a Complete Fertility Picture
No single test tells the whole story. A reproductive endocrinologist—a fertility specialist—acts as a detective, assembling clues from each partner’s results. For example, a woman’s diminished ovarian reserve (low AMH) combined with a man’s borderline low sperm count might point toward a more assertive fertility treatment like In Vitro Fertilization (IVF). Conversely, a simple ovulation issue identified through progesterone testing might be corrected with medication. The power of comprehensive testing lies in integrating these data points to build a holistic diagnosis and a tailored treatment strategy.
At-Home Fertility Tests: Convenience, Limitations, and When to Use Them
The market for direct-to-consumer at-home fertility tests has grown rapidly, offering convenience and privacy. However, it’s crucial to understand their capabilities and limitations.
Types of At-Home Kits Available
At-home options typically include urine-based ovulation predictor kits that track the LH surge, and newer, more complex kits that use blood prick testing (finger prick) to measure key fertility hormones like AMH, FSH, and LH. These might include platforms like the Everlywell app which provides a personal report accessible through a patient account. Basal Body Temperature Charting is another at-home method, though less precise than hormonal tests. For men, some kits offer a basic assessment of sperm count or motility, providing a preliminary screening, though these cannot assess sperm morphology.
Pros and Cons: What At-Home Tests Can & Cannot Tell You (Accuracy & Limitations)
The primary advantage of at-home tests is accessibility. They can provide an early, baseline understanding of certain fertility markers. However, their limitations are significant. While many at-home tests claim 99% accuracy, these statistics typically come from laboratory-controlled settings, not real-world use. Accuracy can vary between 50% to 99% depending on the brand, test type, and proper technique.
Advantages:
-
Convenient and private testing from home
-
Lower initial cost compared to clinical evaluation
-
Can motivate couples to seek professional help
-
Useful for tracking cycles and timing
Limitations:
-
Results lack the clinical context a doctor provides and don’t account for the complete reproductive picture
-
Cannot assess egg quality, ovarian reserve comprehensively, or detect structural abnormalities
-
At-home semen tests cannot assess sperm morphology, a critical factor in sperm function
-
A “normal” result doesn’t guarantee fertility; for example, a normal AMH level doesn’t guarantee fertility if fallopian tubes are blocked
-
Cannot diagnose underlying conditions such as PCOS, endometriosis, or infections
-
Lack of professional interpretation and guidance
-
Timing and adherence to instructions significantly impact accuracy
-
Limited scope means multiple tests may be needed for a more complete picture, increasing costs
Bridging the Gap: When At-Home Results Require Professional Follow-Up and Clinical Diagnosis
At-home fertility tests are best viewed as a screening tool, not a diagnostic one. If an at-home test reveals an abnormal result, or if you still haven’t conceived after the recommended timeframe (12 months if under 35, or 6 months if 35 or older), it is essential to see a fertility specialists or reproductive endocrinologist. A professional will perform validated clinical tests, interpret the results in the context of your full medical history, and provide an accurate diagnosis and fertility treatment plan. Tests performed through certified CLIA laboratories are generally more reliable than rapid at-home tests.
Decoding Your Fertility Test Results: What Do the Numbers Mean?
Receiving a report filled with numbers and acronyms can be confusing. While a specialist is needed for a true interpretation, understanding the basics can be empowering.
Interpreting Female Fertility Test Results
For women, results are often compared to age-specific reference ranges.
Low AMH / High FSH: This combination often suggests a diminished ovarian reserve, meaning a lower quantity of remaining eggs. Women with AMH Levels below 1.0 ng/mL or elevated FSH (above 10 IU/L) may have reduced fertility potential, though pregnancy is still possible.
Abnormal TSH or Prolactin: These results indicate a thyroid or pituitary issue that could be disrupting ovulation and can often be corrected with medication.
Low Mid-Luteal Progesterone: This indicates that ovulation likely did not occur in that cycle, or luteal phase support is insufficient.
Normal AFC but Other Abnormalities: Even with a normal antral follicle count, other factors like egg quality, hormone levels, or structural problems must be investigated.
Interpreting Male Fertility Test Results
Male fertility results are typically compared to World Health Organization (WHO) 2021 reference values.
Low Sperm Count (Oligozoospermia): Fewer than 15 million sperm per milliliter (updated from 15 million/mL in WHO 2010 criteria).
Poor Motility (Asthenozoospermia): Less than 40% total sperm motility or less than 30% progressive motility.
Abnormal Morphology (Teratozoospermia): A high percentage of sperm have an abnormal shape. An abnormal result in one or more areas points to a male factor issue that requires further investigation.
High Sperm DNA Fragmentation: While not part of routine testing, elevated levels may be associated with recurrent pregnancy loss or failed ART cycles.
The Importance of a Reproductive Endocrinologist for Comprehensive Diagnosis
Interpreting fertility test results is a nuanced science. A reproductive endocrinologist—a fertility specialist trained in reproductive medicine—is trained to analyze these complex data sets together, not in isolation. They consider your age, medical history, and physical exam findings to provide a comprehensive diagnosis and guide you toward the most appropriate and effective next steps.
Your Next Steps After Testing: From Results to Action
Getting your test results is not the end of the process; it’s the beginning of an informed action plan.
Discussing Results and Diagnostic Implications with Fertility Specialists
Your follow-up consultation is critical. During this appointment, your specialist will explain what the results mean for you as a couple, answer your questions, and discuss the diagnostic implications. This is your opportunity to gain clarity and understand the potential paths forward. Bring a list of questions and consider bringing your partner for collaborative decision-making.
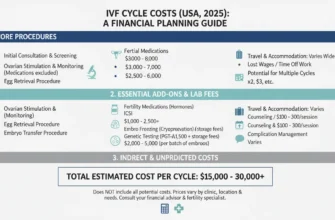
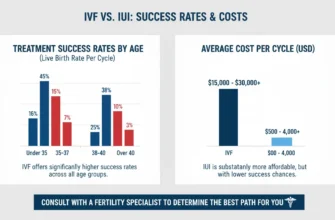
Exploring Fertility Treatment Options (e.g., In Vitro Fertilization – IVF, Assisted Reproductive Technology)
Based on your diagnosis, your doctor will outline potential fertility treatment options. These can range from lifestyle changes and fertility medication (ovulation-inducing medications like clomiphene citrate or letrozole) to more advanced procedures like Intrauterine Insemination (IUI) or In Vitro Fertilization (IVF). Some couples may benefit from ovulation predictor kit use combined with timed intercourse. Test ID documentation and proper lab tests interpretation will inform which assisted reproductive technology approach is most likely to be successful for your specific situation.
The Emotional Aspects of the Fertility Journey and Seeking Support
The fertility testing and treatment process can be emotionally taxing. It is vital to acknowledge these feelings and seek support. This may come from your partner, friends, family, a professional therapist, or support groups of others who are on a similar journey. Prioritizing your mental and emotional well-being is a crucial part of the process. Many fertility clinics now offer counseling services and support resources.
Empowering Your Fertility Path with Knowledge and Action
Fertility testing is a powerful tool that transforms uncertainty into actionable knowledge. By providing a clear, evidence-based understanding of your reproductive health, these lab tests illuminate the path forward. Whether the results lead to simple interventions or more advanced fertility treatments, they are the essential first step toward building your family. Embrace the process as an act of empowerment, and work closely with your fertility specialists to turn your results into a strategic plan for success. Remember that infertility is a treatable condition, and with proper diagnosis and support, many couples can achieve their dreams of parenthood.