Beyond the Odds: Proven Strategies for Successful IVF at 40
Embarking on an in-vitro fertilization (IVF) journey at 40 is a path of profound hope, courage, and strategic decision-making. While conversations often revolve around statistical odds, the reality of modern reproductive medicine is far more nuanced and empowering. Success is not merely a game of chance; it is a result of a proactive, personalized, and multi-faceted approach. The impact of assisted reproductive technology in the United States is substantial, with IVF contributing to 95,860 births in 2023, marking a continued increase in assisted conception success and demonstrating the growing reliability of these treatments. This article moves beyond the statistics to provide a comprehensive guide to the proven strategies that can significantly enhance your chances of building the family you envision.
Understanding the Landscape: IVF at 40+ and the Power of Strategy
Navigating fertility treatment after 40 requires a clear understanding of the biological context and a shift in mindset—from being governed by statistics to being empowered by strategy. This foundational knowledge allows patients to become active participants in their care. The biological realities of advanced maternal age intersect with technological advancement to create new possibilities previously unavailable.
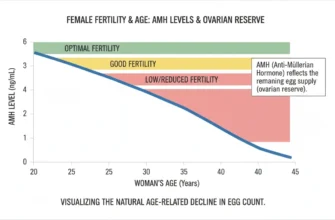
The Biological Realities: Age, Ovarian Reserve, and Egg Quality
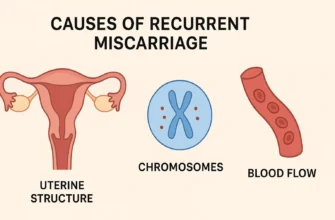
The most significant factor impacting fertility at 40 is the natural decline in both the quantity and quality of eggs. Ovarian reserve, the number of remaining eggs in the ovaries, diminishes with age. More critically, egg quality, which refers to the genetic integrity of an egg, also declines. An older egg is more likely to have chromosomal abnormalities, which can lead to fertilization failure, implantation issues, or an increased risk of miscarriage. This biological reality underscores why assisted reproductive technology (ART) becomes an essential tool for many. The role of the biological clock in fertility decline is well-documented, making strategic intervention increasingly important for women pursuing parenthood after 40.
Shifting the Focus: From “Odds” to “Actionable Strategies”
While statistics provide a general framework, they do not define an individual’s potential outcome. The most productive approach is to shift focus from static odds to dynamic, actionable strategies. This means concentrating on controllable factors: choosing the right fertility clinics, undergoing comprehensive diagnostic testing, optimizing lifestyle, and collaborating with your fertility specialist on a tailored treatment plan. Success is built through a series of well-informed decisions and medical interventions designed to maximize every opportunity within an IVF cycle.
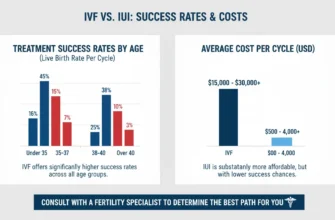
Setting Realistic Expectations While Cultivating Hope for Live Birth Rates
It’s crucial to balance optimism with realism. For women between 38 and 40, general IVF success rates show clinical pregnancy rates around 20-30% per cycle. However, this is not the end of the story. Cumulative live birth rate is a key concept; many patients require more than one IVF cycle. A 2024 study revealed that after multiple transfers, women aged 40 have a cumulative live birth rate of 55.6%, demonstrating the importance of multiple gestation planning and persistence. This highlights the importance of persistence and strategic planning for multiple cycles, transforming the journey from a single sprint into a thoughtfully paced marathon.
Strategic Foundations: Comprehensive Assessment and Personalized Treatment Protocols
A successful IVF journey at 40 is built upon a foundation of meticulous planning and personalization. Generic, one-size-fits-all approaches are insufficient; success depends on a treatment plan that is precisely tailored to your unique biological landscape. Working with experienced fertility specialists and utilizing advanced diagnostics forms the foundation of success.
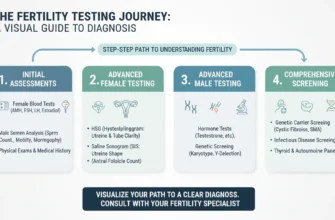
A. Unveiling Your Unique Fertility Profile: Advanced Diagnostics
Before beginning any fertility treatment, a thorough diagnostic workup is essential. This goes beyond basic blood tests and includes:
Ovarian Reserve Testing: Measuring Anti-Müllerian Hormone (AMH) and Follicle-Stimulating Hormone (FSH) levels, along with an antral follicle count via ultrasound, provides a clear picture of your remaining egg supply and guides cycle regulation strategies. Hormone levels are critical indicators of ovarian function and response potential.
Uterine Evaluation: A saline infusion sonogram (SIS) or hysteroscopy is used to examine the uterine cavity for polyps, fibroids, or scar tissue that could interfere with embryo implantation. These structural evaluations are essential for preparing the womb lining for transfer.
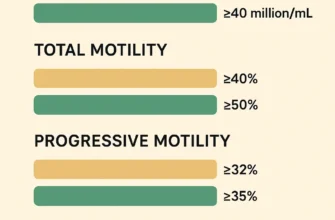
Sperm Analysis: Male factor infertility is a significant component. Research demonstrates that men aged 40 and above can experience declining sperm quality, which impacts fertility treatment outcomes. A comprehensive semen analysis assesses sperm count, motility, and morphology. Studies show that sperm quality declines with maternal age of the partner, particularly after age 40, where reductions in total sperm motility and progressive motility become pronounced.
B. Tailored Ovarian Stimulation Protocols: Maximizing Egg Quality and Quantity
The goal of ovarian stimulation is to encourage the ovaries to produce multiple mature eggs for egg retrieval. For patients over 40, protocols are often adjusted to prioritize egg quality over sheer quantity. Strategies may include:
Microdose Lupron or “Flare” Protocols: These can help recruit a more synchronized cohort of follicles in patients with diminished ovarian reserve, optimizing follicular development.
Antagonist Protocols: These offer flexibility and can reduce the risk of Ovarian Hyperstimulation Syndrome (OHSS), while effectively preventing premature ovulation. These ovarian stimulation drugs represent advances in assisted conception.
Adjuvant Therapies: Some protocols may incorporate supplements like Coenzyme Q10 (CoQ10) or growth hormone, though their efficacy is still debated and should be discussed with your healthcare provider. Emerging therapies like Platelet Rich Plasma (PRP) and Mesenchymal Stem Cells (MSCs) are under investigation for their potential to improve ovarian response, though evidence remains preliminary.
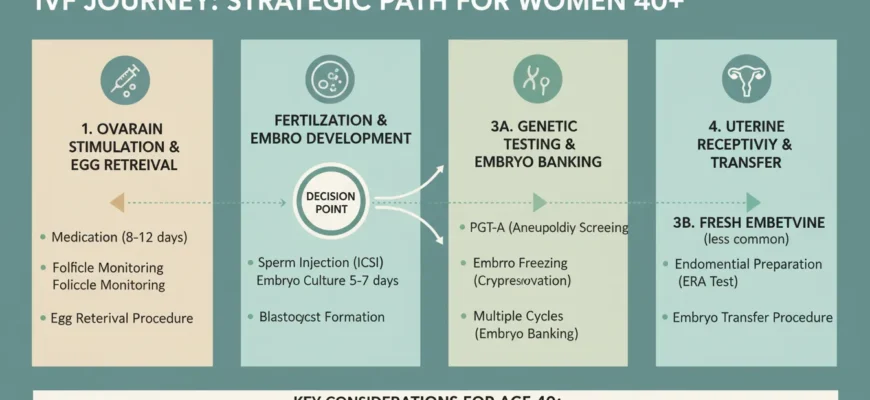
Optimizing Embryo Development and Selection: The Core of Successful IVF Cycles
Once eggs are retrieved, the focus shifts to the embryology lab, where the most critical stages of development occur. Advanced techniques in this phase are paramount for success. The quality of embryo development directly impacts pregnancy success rates and the likelihood of achieving a live birth rate.
A. Advanced Embryology Techniques: Cultivating Healthy Embryos
The journey from egg to embryo requires a highly controlled environment and expert techniques. Intracytoplasmic sperm injection (ICSI), where a single, healthy sperm is injected directly into an egg, is a common procedure particularly beneficial in cases of male factor infertility. Research shows that ICSI has become increasingly utilized in modern stimulated cycles. Embryos are then cultured for 5-6 days to the blastocyst embryo stage in specialized incubators that mimic the uterine environment. This extended culture period allows for better selection of developmentally competent embryos.
B. The Power of Preimplantation Genetic Testing for Aneuploidy (PGT-A)
Preimplantation genetic testing (PGT-A)—also referred to as Preimplantation genetic testing for aneuploidy (PGT-A) or pre-implantation genetic screening—is one of the most significant advancements for improving IVF outcomes in women over 40. This genetic screening technology involves taking a small biopsy from a blastocyst embryo to test for the correct number of chromosomes. By identifying chromosomally normal (euploid) embryos, PGT-A helps to:
-
Increase the chance of implantation per transfer
-
Reduce the rate of miscarriage, which is often caused by genetic abnormalities and chromosomal abnormalities
-
Decrease the time to achieve pregnancy by avoiding the transfer of non-viable embryos
For women aged 38 to 40, PGT-A testing results in an implantation rate of approximately 61.1% compared to just 32.9% without it, representing a significant improvement in outcomes. This technology is particularly valuable when combined with elective single embryo transfer strategies to optimize safety while maintaining high success rates.
C. Embryo Banking and Freezing: Building a Reserve for Cumulative Success
Given that a single IVF cycle may not yield enough normal embryos, embryo banking is a powerful strategy. This involves undergoing multiple egg retrieval cycles to collect and freeze several euploid embryos before proceeding to an embryo transfer. Embryo freezing through vitrification system methods preserves embryo viability effectively. This approach maximizes the potential of each retrieval, builds a reserve for future frozen embryo transfers (FETs), and increases the cumulative live birth rate over time without the pressure of a ticking biological clock for each subsequent attempt. Embryo vitrification has become the gold standard for cryopreservation, offering superior survival rates compared to traditional slow-freezing methods.
Enhancing Implantation: Preparing the Uterus for Embryo Transfer
Creating a healthy embryo is only half the battle. The uterus must be optimally prepared to receive it. This involves careful monitoring and interventions to ensure the uterine lining is receptive, maximizing the chances of successful implantation and pregnancy test positivity.
A. Optimizing the Endometrial Environment: Receptivity of the Womb Lining
A successful embryo transfer depends on a receptive endometrium (uterine lining). This is achieved through hormonal support, typically with estrogen and progesterone, to ensure the lining is of adequate thickness and structure. For frozen embryo transfers (FETs), a “programmed” or “medicated” cycle allows for precise control over the timing, ensuring the womb lining is perfectly synchronized with the embryo’s developmental stage. The quality of the endometrial environment is critical for successful implantation and sustained pregnancy development.
B. Addressing Recurrent Implantation Failure and Reproductive Immunology
For patients who have experienced multiple failed transfers with high-quality embryos, further investigation may be necessary. Recurrent implantation failure (RIF) can be caused by underlying issues such as chronic endometritis, uterine structural problems, or immunological factors. Tests for blood clotting disorders or an Endometrial Receptivity Array (ERA) may be considered. The Endometrial Receptivity Analysis can help identify a displaced window of implantation in selected cases.
Reproductive immunology is an emerging field that explores how the maternal immune system interacts with the embryo, offering potential treatments for select cases. Understanding autoimmune issues and their relationship to implantation failure represents an important frontier in treating recurrent failure. Emerging treatments include Mesenchymal Stem Cells and other immune-modulating approaches, though evidence remains under investigation.
Considering Third-Party Reproduction: Expanding Pathways to Parenthood
When using one’s own eggs presents significant challenges, third-party reproduction offers highly effective and fulfilling paths to building a family. It is a strategic choice that empowers patients with more options for achieving parenthood.
A. When to Consider Donor Eggs: A Highly Successful Strategy
For many women over 40, especially those with severely diminished ovarian reserve or who have had multiple unsuccessful IVF cycles, using donor eggs can dramatically increase the chances of success. The live birth rate is based on the age of the egg donor, not the recipient. For women over 43, egg donors are often the most reliable option, with donor eggs achieving success rates exceeding 35% per transfer. This is significantly higher than the 5% or lower success rates typical when using one’s own eggs at this age.
The Society for Assisted Reproductive Technology (SART) and American Society for Reproductive Medicine (ASRM) data consistently demonstrate that egg sharing and traditional egg donation programs achieve pregnancy success rates of 50-70% per embryo transfer, with cumulative live birth rates reaching 75-95% across multiple cycles. This path allows a woman to carry the pregnancy and give birth, providing a powerful biological connection to her child. The use of donor eggs transforms fertility prospects for advanced maternal age patients, making assisted conception viable well into the 40s and beyond.
B. Donor Sperm and Surrogacy: Additional Options for Family Building
If male factor infertility is severe or for single women and same-sex couples, donor sperm is a widely used and successful option. In cases where a woman cannot carry a pregnancy due to uterine factors or medical conditions, gestational diabetes or other health concerns may be managed through a surrogate. Gestational surrogacy—using a carrier to carry an embryo created from the intended parents’ (or donors’) gametes—provides another viable route to parenthood. These options continue to expand access to reproductive treatment for diverse family structures and circumstances.
Lifestyle and Wellness: Supportive Pillars for Your IVF Journey
While medical technology is the cornerstone of IVF, a holistic approach that includes lifestyle and wellness can create the best possible foundation for treatment. Optimizing overall health supports both the biological requirements of fertility treatment and the emotional resilience needed to navigate the journey.
A. Nutrition for Fertility: Evidence-Based Dietary Choices
A nutrient-dense diet rich in antioxidants, healthy fats, and whole grains can support reproductive health. A Mediterranean-style diet, with its emphasis on fruits, vegetables, fish, and olive oil, has been associated with improved fertility outcomes in multiple studies. Research shows that women with higher adherence to a Mediterranean diet had 65-68% greater likelihood of achieving successful pregnancy and live birth rates during assisted conception compared to those with lowest adherence. Limiting processed foods, excessive sugar, and caffeine is also advisable. The Mediterranean-style diet represents an evidence-based nutritional approach specifically validated for improving IVF success outcomes.
B. Stress Management and Emotional Well-being: Nurturing Mind and Body
The IVF process is emotionally demanding. Chronic stress can impact hormonal balance, making stress management crucial. Practices like mindfulness, yoga, meditation, and gentle exercise can help regulate the nervous system. Prioritizing sleep is also essential for both physical and emotional resilience during the demanding treatment schedule. Autoimmune issues and stress-related conditions can be exacerbated during fertility treatment, making emotional support particularly important.
C. Physical Activity and Environmental Factors
Moderate physical activity is beneficial for circulation and stress reduction, but high-intensity exercise should be avoided during the stimulation and post-transfer phases. It is also wise to minimize exposure to endocrine-disrupting chemicals found in some plastics, pesticides, and personal care products. Supporting natural pregnancy foundations through environmental optimization creates synergy with medical interventions.
The Emotional and Psychological Journey: Building Resilience Through IVF at 40
The path of IVF is as much an emotional marathon as it is a medical one. Acknowledging and preparing for the psychological challenges is a critical component of a successful and sustainable journey. Understanding the emotional landscape helps patients and partners navigate the experience with greater awareness and compassion.
Navigating the Emotional Rollercoaster: Hope, Anxiety, and Disappointment
Fertility treatment involves cycles of intense hope followed by periods of anxious waiting, and potentially, deep disappointment. The failure of an IVF cycle can be devastating. A landmark 1988 study found that 94% of women and 64% of men experienced depressive symptoms after a first failed round of IVF treatment. More recent research confirms that psychological distress is common following unsuccessful cycles, with both depression and anxiety being significant concerns. Recognizing these feelings as a normal part of the process is the first step toward managing them. The emotional intensity of recurrent IVF failure can be particularly challenging, requiring specialized support strategies.
The Importance of a Strong Support System: Partner, Family, and Friends
Lean on your support network. Open communication with your partner is vital, as you are both navigating this experience. Inform trusted family members or friends who can offer empathy and practical support without judgment. Connecting with others who have gone through IVF can also provide an invaluable sense of community and understanding. Peer support groups, whether online or in-person, can reduce isolation and provide practical coping strategies.
Seeking Mental Health Support: Therapists Specializing in Fertility
Professional support is a sign of strength. Therapists who specialize in fertility can provide coping strategies, communication tools, and a safe space to process the complex emotions that arise during treatment. Many fertility clinics have mental healthcare providers on staff or can provide referrals to specialists trained in fertility-related mental health. Some clinics now offer video call consultations with mental health professionals, improving accessibility to specialized support.
Building Resilience and Practicing Self-Care During Treatment
Resilience is built by practicing self-compassion. Give yourself permission to feel what you feel, set boundaries to protect your emotional energy, and schedule non-fertility-related activities that bring you joy. Self-care isn’t an indulgence; it’s a necessary component of enduring the rigors of treatment. Developing personalized coping strategies before beginning treatment can provide anchoring tools when emotional challenges arise.
Choosing Your IVF Team and Clinic: A Critical Decision for Success
The expertise of your medical team and the quality of the fertility clinics are arguably among the most important factors in your journey. This is where you place your trust, hope, and resources. Careful clinic selection can significantly impact your treatment outcomes and overall experience.
A. What to Look for in a Fertility Clinic and Specialist
Look for a clinic with extensive experience treating patients over 40. Scrutinize their success rates, particularly their live birth rates for your age group, which are often reported to organizations like the Society for Assisted Reproductive Technology (SART). According to the Centers for Disease Control and Prevention (CDC) and National Assisted Reproductive Technology Surveillance System (NASS), reliable clinics maintain transparent reporting of outcomes. A high-quality embryology lab is non-negotiable—inquire about laboratory accreditation and embryologist experience with older patients.
Crucially, choose a fertility specialist who communicates clearly, respects your input, and customizes your treatment plan. Ask about their use of advanced diagnostics like Endometrial Receptivity Analysis and preimplantation genetic testing in their protocols. Understanding their approach to recurrent implantation failure and experience with advanced maternal age populations is essential. Some clinics may utilize tools like the IVF Success Estimator to provide personalized outcome predictions based on your specific profile.
B. Becoming Your Own Advocate: Informed Decision-Making
The best patient is an informed patient. Ask questions, research your options, and understand the rationale behind every step of your treatment plan. Feel empowered to seek a second opinion if you feel unheard or uncertain. Request data from multiple clinics and compare not just success rates but also their approach to personalized treatment protocols. Understand the difference between natural cycle IVF and stimulated approaches, and know which may be appropriate for your circumstances.
Your active participation in decision-making ensures that the chosen path aligns with your goals, values, and personal circumstances. Request information about their experience with twin pregnancy outcomes if elective single embryo transfer is being considered versus double embryo transfer. Understanding all options, from fresh embryo transfer to frozen embryo transfer, allows you to make informed choices alongside your medical team.
Laboratory Considerations: Supporting Excellence in Embryology
The embryology lab is where the critical work of creating viable embryos occurs. Modern labs employ time-lapse imaging systems and advanced embryo culture protocols to optimize development. For older patients, the quality of laboratory conditions becomes even more critical, as aging oocytes are more sensitive to environmental stressors. Understanding your clinic’s laboratory practices, including their incubator technology, culture media selection, and embryo assessment protocols, provides important insights into expected outcomes.
Advanced facilities may offer specialized services for challenging cases, such as in vitro maturation (IVM) of immature eggs or rescue protocols for fertilization failure. For patients with severe male factor infertility, Intracytoplasmic sperm injection (ICSI) availability and expertise with difficult cases demonstrates laboratory sophistication.
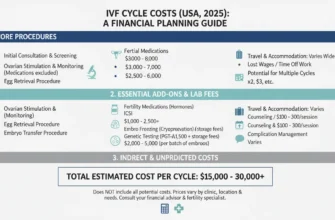
Navigating Treatment Costs and Insurance Coverage
Fertility drugs and comprehensive IVF treatment represent significant financial investments. Understanding medication costs, clinic fees, and insurance coverage is essential for planning. Some fertility medications may be available through patient assistance programs. The American Society for Reproductive Medicine (ASRM) and Center for Disease Control (CDC) provide guidance on navigating insurance advocacy. Many patients find working with a fertility specialist who understands insurance requirements helpful in maximizing coverage and minimizing unexpected costs.
Moving Forward: A Realistic and Hopeful Perspective
IVF at 40 is not an impossible dream—it is a navigable path with significantly improved odds when approached strategically. The combination of advanced reproductive medicine, personalized treatment plans, and comprehensive support creates a compelling framework for success. While biological realities demand respect and realistic expectations, the tools now available represent genuine breakthroughs in assisted reproduction.
Key takeaways for your journey:
Prioritize comprehensive diagnostics to understand your unique fertility profile. Optimize lifestyle factors including diet, stress management, and environmental exposures. Invest in quality medical care from experienced fertility specialists and high-functioning clinics. Utilize advanced technologies like PGT-A to select the best embryos. Plan for multiple cycles and understand cumulative live birth rates rather than single-cycle odds. Embrace emotional support as integral to treatment success. Remain flexible regarding third-party reproduction options if needed.
Conclusion
Successfully navigating IVF at 40 is about moving “beyond the odds” and embracing a strategic, proactive, and personalized approach. It requires acknowledging the biological clock and the biological realities of advanced maternal age while focusing on the powerful tools of modern reproductive medicine. From advanced diagnostics and tailored protocols to cutting-edge embryology with PGT-A and considering all pathways to parenthood, every decision is a step toward your goal. By supporting this medical journey with robust emotional care, healthy lifestyle choices anchored in evidence-based approaches, and a trusted medical team, you empower yourself to face the challenges with resilience and hope.
The path may be complex, and success is not guaranteed, but with the right strategies, support, and medical guidance, building your family after 40 is a tangible and increasingly achievable reality. The combination of fertility treatment advances, personalized treatment protocols, and comprehensive support represents genuine hope for those pursuing parenthood at this life stage.