Understanding Male Fertility and Reproductive Function
The Importance of Sperm Quality in Conception
Conception requires a true biological partnership. For successful fertilization to occur, healthy sperm must navigate through the female reproductive tract and successfully penetrate an egg. This demanding journey requires not just a sufficient number of sperm, but sperm of exceptional quality. The structure, motility, and functional capacity of sperm are paramount to achieving successful fertilization and supporting healthy embryo development through the blastocyst stage.
Evaluating male fertility is not simply about identifying problems—it is about proactively optimizing the biological conditions for conception. Understanding semen parameters and reproductive function provides the foundational data needed to assess fertility potential and guide any necessary interventions. Male factors contribute to infertility in approximately 50% of couples, making knowledge of sperm parameters—including sperm count, sperm quality, sperm motility, and other semen parameters—essential for any couple seeking to conceive.
What This Guide Covers: Moving Beyond “Normal” to “Optimal”
This comprehensive guide examines the crucial semen parameters that influence pregnancy outcomes and reproductive outcomes. We will decode what a semen analysis report means, explaining the World Health Organization (WHO) criteria and reference limits for evaluating sperm analysis results. More importantly, we will explore the critical distinction between “normal” and “optimal” sperm quality. We’ll examine the major factors affecting spermatogenesis and sperm production—from lifestyle to environmental exposures—and provide evidence-based strategies to enhance male fertility. The goal is to empower readers with actionable knowledge to take control of reproductive function on the path to parenthood.
Understanding Your Semen Analysis Report: WHO Guidelines and Benchmarks
What is a Semen Analysis?
A semen analysis is the cornerstone of male fertility evaluation. It is a laboratory test that measures the quantity and quality of a man’s semen and the sperm contained within it. This non-invasive analysis provides a detailed snapshot of reproductive health, evaluating several critical semen parameters simultaneously. For patients beginning their fertility journey, this sperm analysis report is often the first and most informative step, offering crucial insights into the male partner’s contribution to the couple’s overall fertility potential. The results from the sperm analysis are compared against established WHO reference values to identify any areas requiring attention or improvement.
Key Semen Parameters According to WHO 2021 Criteria
The World Health Organization released its 6th edition of the Laboratory Manual for the Examination and Processing of Human Semen in July 2021, providing updated, standardized, evidence-based procedures for semen analysis worldwide. These WHO criteria are used by andrology laboratories globally to ensure consistent and reliable testing. The main semen parameters include:
Sperm Concentration (Sperm Density): This is the number of sperm per milliliter (mL) of semen. The WHO 2021 lower reference limit is 16 million sperm/mL (previously 15 million/mL in 2010 guidelines). This represents the 5th percentile reference value based on data from fertile men.
Total Sperm Count: This measures the total number of sperm in the entire ejaculate. The WHO 2021 benchmark is 39 million or more per ejaculate.
Semen Volume: The total amount of semen ejaculated. According to WHO 2021, a normal volume is considered 1.4 mL or more (previously 1.5 mL in the 2010 guidelines). The seminal plasma contains important components from the seminal vesicles, prostate gland, and bulbourethral glands that support sperm survival and function.
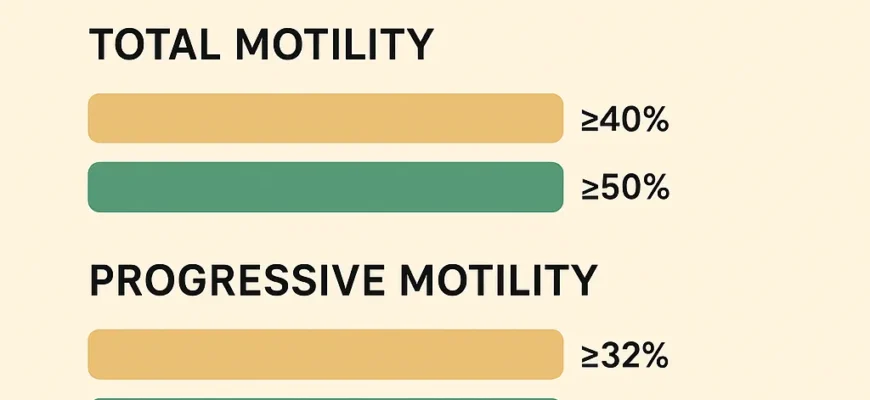
Sperm Motility: This refers to the ability of sperm to move, which is critical for reaching and fertilizing the egg. The WHO criteria distinguish between several types:
-
Total Motility: The percentage of all moving sperm (both progressive and non-progressive). WHO 2021 reference: 42% or more
-
Progressive Motility: The percentage of sperm moving forward in a straight line or large circles. This is the most critical form of motility for achieving fertilization. WHO 2021 reference: 30% or more (previously 32% in 2010)
-
Rapid Progressive Motility: Sperm moving swiftly and efficiently, covering at least half the length of their tail each second
-
Slow Progressive Motility: Sperm moving forward at slower pace but still purposefully
-
Non-Progressive Motility: Sperm moving but without forward progress
-
Immotile Sperm: Sperm with no active movement; some immotile sperm is normal
The Total Motile Count (TMC): This is calculated by multiplying sperm concentration × semen volume × percentage of total motility. A total motile count of over 20 million is considered normal and is one of the most important parameters for fertility potential.
Morphology (Sperm Shape): The size and shape of sperm cells. Normal morphology, with at least 4% of sperm having a normal shape, is associated with better fertilization potential. Men with poor morphology have abnormal sperm morphology, which may reduce fertilization ability. However, even with low normal morphology percentages, pregnancy can still occur if other parameters are adequate.
Sperm Vitality: The percentage of live sperm in the sample. According to WHO criteria, at least 54% of sperm should be alive.
Interpreting Your Sperm Analysis Report
Receiving a semen analysis report can seem overwhelming, but understanding the values is straightforward. Here’s what various results mean:
If your sperm concentration is 20 million/mL, this is above the WHO 2021 reference limit of 16 million/mL and is considered normal. Similarly, progressive motility of 35% exceeds the 30% minimum. It is crucial to remember that these WHO reference values represent the lower reference limits—the 5th percentile in fertile men—not guarantees of fertility.
Falling below the reference limits in one or more parameters may indicate a potential issue:
-
Oligospermia (low sperm count): Total sperm count below 39 million
-
Oligozoospermia (low sperm concentration): Below 16 million/mL
-
Asthenozoospermia (poor motility): Progressive motility below 30%
-
Teratozoospermia (poor morphology): Less than 4% normal forms
-
Hypospermia (low volume): Less than 1.4 mL
-
Azoospermia (no sperm): Complete absence of sperm in the ejaculate
-
Virtual Azoospermia (extremely low count making natural conception virtually impossible)
-
Idiopathic Oligoasthenoteratozoospermia (OAT): Combined defects in count, motility, and morphology with no identified cause
These conditions warrant further discussion with a fertility specialist.
Beyond “Normal”: Understanding Optimal Sperm Quality for Enhanced Fertility
The Difference Between “Normal” and “Optimal”
The WHO guidelines define the minimum threshold required for a man to be considered potentially fertile, but they do not define the ideal range for maximizing fertility. “Normal” means you meet the baseline; “optimal” means your parameters are in a range that significantly increases the probability of natural conception.
For instance, while 16 million sperm/mL is “normal,” research demonstrates that men with sperm concentrations above 40 million/mL have notably higher pregnancy rates. Similarly, total motility of 42% is technically normal, but studies show that progressively higher motility rates correlate with improved fertilization rates and reproductive outcomes.
Optimal fertility involves not just meeting but substantially exceeding these minimums. Striving for optimal sperm quality improves the overall reproductive function of sperm, enhancing their ability to achieve fertilization and support healthy blastocyst stage development. This is particularly important in natural conception scenarios where competition among millions of sperm determines which reaches the egg first.
How Suboptimal Parameters Impact Fertilization Success
Even if sperm parameters fall within the “normal” range according to WHO criteria, suboptimal values can still present challenges for conception:
-
Low-normal sperm count reduces the total number of viable candidates available to fertilize the egg, decreasing the odds of successful fertilization each cycle
-
Poor progressive motility means fewer sperm will complete the arduous journey through the female reproductive tract to reach the fallopian tube and egg
-
Poor morphology can hinder the sperm’s ability to penetrate the egg’s outer layers
-
Low volume may provide insufficient seminal plasma to support sperm during their journey
-
Low vitality means more dead sperm in the ejaculate, reducing functional sperm available for fertilization
The interaction between parameters is equally important. A high sperm count is far less effective if the volume is very low, if motility is poor, or if morphology is abnormal. Each parameter plays an interconnected role in reproductive function, and deficiencies in any area can substantially lower the monthly probability of successful fertilization.
Major Factors Affecting Sperm Production, Sperm Quality, and Male Fertility
Oxidative Stress and Reactive Oxygen Species (ROS)
Oxidative stress is a critical contributor to male infertility. It occurs when there is a dangerous imbalance between reactive oxygen species (ROS) and antioxidant defenses in the body. Sperm cells are particularly vulnerable to ROS damage because their cell membranes are rich in polyunsaturated fatty acids, making them susceptible to lipid peroxidation and oxidative damage.
ROS-mediated damage affects male fertility through multiple mechanisms:
-
DNA Damage: ROS can cause sperm DNA integrity impairment, including DNA strand breaks and fragmentation
-
Sperm Motility Impairment: Oxidative damage to the cell membrane and mitochondria reduces sperm movement
-
Morphological Defects: ROS damage can prevent normal sperm shape development
-
Decreased Sperm Concentration: High ROS levels can trigger programmed cell death (apoptosis) in developing germ cells during spermatogenesis
Research indicates that oxidative stress-associated DNA damage is found in 30–80% of infertile males, representing a major yet often overlooked cause of male infertility.
Common sources of elevated ROS include:
-
Environmental pollution and toxins
-
Smoking and tobacco use
-
Excessive alcohol consumption
-
Poor diet lacking antioxidants
-
Chronic stress and elevated cortisol
-
Bacterial and viral infections
-
Varicocele (discussed below)
-
Obesity and metabolic dysfunction
Total Antioxidant Capacity and the Body’s Defense System
The body produces several enzymatic antioxidants to combat oxidative stress:
-
SOD (Superoxide Dismutase) Activity: Converts superoxide radicals to hydrogen peroxide
-
CAT (Catalase) Activity: Breaks down hydrogen peroxide to water and oxygen
-
Glutathione Peroxidase: Protects against lipid peroxidation
The Total Antioxidant Capacity (TAC) of seminal plasma reflects the combined antioxidant status and is increasingly recognized as an important marker of male fertility potential. Men with compromised antioxidant systems are at higher risk for compromised semen quality.
Hormonal Imbalances and Spermatogenesis
Sperm production (spermatogenesis) is a complex, 74-day process regulated by a delicate hormonal balance. This involves three main hormones:
Testosterone: The primary male sex hormone, essential for all stages of sperm development. Testosterone is produced by Leydig cells in response to luteinizing hormone (LH). An imbalance in testosterone levels directly affects sperm production and quality.
Follicle-Stimulating Hormone (FSH): Stimulates Sertoli cells in the seminiferous tubules to support spermatogenesis. Elevated FSH often indicates germinal epithelial damage or spermatogenic failure.
Luteinizing Hormone (LH): Signals Leydig cells to produce testosterone, which is required for completing spermatogenesis.
Hormonal conditions affecting male fertility include:
-
Hypogonadism (Low Testosterone): Can severely reduce sperm production
-
Thyroid Disorders: Thyroid hormones regulate metabolic processes essential for reproductive function. Both hypothyroidism and hyperthyroidism impair spermatogenesis
-
Hyperprolactinemia: Elevated prolactin suppresses GnRH (gonadotropin-releasing hormone), reducing FSH and LH production
-
Pituitary Dysfunction: Affects production of FSH and LH, disrupting the hypothalamic-pituitary-gonadal (HPG) axis
A healthcare provider can assess hormone levels through blood tests to determine if they contribute to fertility issues.
Lifestyle Factors: Diet, Exercise, Stress, and Sleep
Everyday choices profoundly impact male fertility and semen parameters:
Diet and Nutrition:
-
A diet lacking in antioxidants, vitamins, and minerals fails to protect sperm from oxidative damage
-
Conversely, a diet rich in antioxidants, fruits, vegetables, lean proteins, and healthy fats supports robust sperm health
-
Zinc (found in oysters, beef, pumpkin seeds) is essential for sperm formation and testosterone metabolism
-
Selenium (in Brazil nuts and fish) is crucial for sperm motility and antioxidant enzyme function
-
Vitamin C and E protect sperm from oxidative damage
-
Coenzyme Q10 (CoQ10) improves energy production in sperm mitochondria and acts as a powerful antioxidant
-
Folic acid deficiency is associated with abnormal sperm morphology
Exercise:
-
Regular, moderate exercise (150+ minutes per week) boosts testosterone levels and improves semen parameters
-
Excessive or high-intensity exercise can paradoxically decrease testosterone and harm fertility
-
Sedentary behavior is linked to increased infertility risk
Smoking, Alcohol, and Drugs:
-
Smoking is one of the most detrimental habits for sperm health, strongly linked to decreased sperm count, motility, and morphology
-
Excessive alcohol consumption negatively impacts testosterone levels and semen quality
-
Illicit drugs impair spermatogenesis and fertility
Stress and Sleep:
-
Chronic stress elevates cortisol, which suppresses reproductive hormones and increases ROS production
-
Inadequate sleep (<7 hours per night) disrupts hormonal regulation, increases oxidative stress, and reduces testosterone
-
Stress-reduction techniques like meditation, yoga, and deep breathing support fertility
Body Weight:
-
Obesity negatively alters hormone levels, increases oxidative stress, and raises scrotal temperature, all of which harm sperm production
-
Underweight conditions can also compromise testosterone production and sperm quality
-
Maintaining a healthy BMI supports optimal reproductive function
Testicular Temperature and Heat Stress
The testicles require a temperature 3.5–7°F (1.9–3.9°C) cooler than core body temperature for optimal spermatogenesis. Elevated scrotal temperatures cause multiple fertility problems:
Mechanisms of Heat-Induced Damage:
-
Testicular Hyperthermia: Elevated scrotal temperature impairs sperm development at multiple stages
-
Oxidative Stress: Heat increases ROS production in testicular tissue
-
DNA Damage: Heat-induced DNA damage in developing spermatocytes and spermatids can cause sperm DNA integrity problems
-
Apoptosis (Cell Death): Heat triggers programmed cell death in germ cells
-
Mitochondrial Dysfunction: Heat damages the mitochondrial bioenergetics machinery that powers sperm movement
Common Heat Exposure Sources:
-
Hot tubs, saunas, and hot-water baths: Even short periods can raise scrotal temperature to dangerous levels
-
Tight underwear: Reduces air circulation; choose loose-fitting boxers instead of briefs
-
Laptop use: Placing a laptop directly on your lap increases scrotal temperature by 0.6–0.8°C
-
Heated car seats: Extended use (>60 minutes) can add 0.5–0.6°C increase
-
Occupational heat exposure: Welders, bakers, and others in hot environments face higher infertility risk
-
Manual work in tropical climate: Outdoor laborers in high-temperature environments experience reduced sperm quality
-
Prolonged sitting with legs together: Increases scrotal temperature approximately 2.1°C
Recovery Timeline: If heat exposure is discontinued, sperm counts typically improve within 4–12 weeks, though full recovery may take longer.
Medical Conditions Affecting Sperm Health and Reproductive Outcomes
Varicocele: An enlargement of the veins within the scrotum, varicocele is the most common treatable cause of male infertility, affecting approximately 15–20% of men. It causes:
-
Elevated scrotal temperature
-
Increased oxidative stress and ROS production
-
Impaired sperm production
-
Higher sperm DNA fragmentation rates
-
Reduced testosterone production
Surgical repair (microsurgical varicocelectomy) can significantly improve semen parameters and reduce sperm DNA fragmentation, with studies showing pregnancy rates of 20–40% within one year after repair.
Infections: Bacterial, viral, or parasitic infections of the reproductive tract can impair sperm production and motility through inflammatory pathways and oxidative stress.
Genetic Conditions:
-
Klinefelter Syndrome (47, XXY): The most common genetic cause of male infertility, resulting in non-obstructive azoospermia (no sperm production). Characterized by small testes, low testosterone, and elevated FSH. Despite this, some men with Klinefelter syndrome may have rare sperm in ejaculate or retrievable testicular sperm suitable for intracytoplasmic sperm injection (ICSI).
-
Y-Chromosome Microdeletions: Deletions in azoospermia factor (AZF) regions impair spermatogenesis
Structural Blockages: The vas deferens, epididymis, or ejaculatory ducts can become blocked, preventing sperm from being ejaculated (obstructive azoospermia). Unlike non-obstructive azoospermia, sperm production may be normal, but sperm cannot reach the semen.
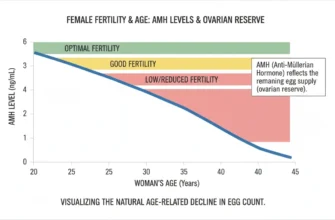
Age-Related Decline: Sperm quality gradually declines after age 40, with studies showing:
-
Progressive decline in sperm motility starting around age 35, with significant decreases after 40
-
Increased DNA fragmentation after age 40
-
Higher risk of sperm DNA damage and oxidative stress
-
Increased risk of birth defects and miscarriage in offspring
-
Reduced testosterone production with advancing age
Strategies for Optimizing Sperm Health: Actionable Steps for Enhanced Male Fertility
Dietary Optimization: The Power of Antioxidants and Micronutrients
Your diet is one of the most powerful tools for improving sperm health and male fertility. Antioxidants are critical for neutralizing the damaging effects of ROS. Focus on incorporating foods rich in key nutrients:
Antioxidant-Rich Foods:
-
Citrus fruits and berries (vitamin C sources)
-
Leafy green vegetables (folate, vitamins)
-
Nuts and seeds (vitamin E, selenium, zinc)
-
Fatty fish (omega-3 fatty acids, selenium)
Specific Micronutrient Sources:
-
Zinc (oysters, beef, pumpkin seeds, cashews): Essential for sperm formation, morphology, and testosterone metabolism
-
Selenium (Brazil nuts, fish, poultry): Crucial for sperm motility and antioxidant enzyme function
-
Vitamin C (oranges, kiwis, peppers): Protects sperm from oxidative damage and improves motility
-
Vitamin E (almonds, sunflower seeds): Powerful fat-soluble antioxidant protecting sperm membranes
-
Coenzyme Q10 (beef, fish, nuts): Improves sperm energy production and reduces sperm DNA fragmentation
Healthy Fats:
-
Omega-3 fatty acids support sperm cell membrane integrity
-
Mediterranean diet patterns correlate with improved semen parameters
-
Avoid trans fats and excessive saturated fats
Hydration:
-
Proper hydration supports semen volume and sperm concentration
-
Adequate water intake aids toxin elimination
Lifestyle Adjustments for Enhanced Sperm Quality
Simple lifestyle modifications can yield significant improvements in semen parameters:
Weight Management:
-
Maintain a healthy BMI (18.5–24.9)
-
Obesity reduces testosterone and impairs spermatogenesis
-
Even modest weight loss (5–10%) can improve semen parameters
Physical Activity:
-
Aim for 150 minutes of moderate-intensity aerobic activity per week
-
Include resistance training 2–3 times per week
-
Avoid excessive endurance training (>15 hours/week)
-
Regular exercise boosts testosterone and improves blood flow to reproductive organs
Smoking Cessation:
-
Smoking is one of the most detrimental habits for sperm health
-
Quitting leads to noticeable improvements in sperm count and motility within 2–3 months
-
Complete recovery of semen parameters may take 6–12 months
Limit Alcohol and Caffeine:
-
Excessive alcohol consumption (>3 drinks per day) negatively impacts testosterone and semen quality
-
Moderate caffeine consumption is generally acceptable
-
Avoid binge drinking
Stress Management:
-
Practice stress-reduction techniques such as:
-
Meditation and mindfulness
-
Yoga
-
Deep breathing exercises
-
Regular physical activity
-
Adequate sleep
-
Counseling or therapy
-
Optimize Sleep:
-
Aim for 7–9 hours of quality sleep nightly
-
Maintain consistent sleep schedules
-
Sleep deprivation reduces testosterone and increases cortisol and oxidative stress
Environmental Protection: Minimizing Exposure to Testicular Threats
Protecting sperm from environmental damage requires awareness and behavioral modifications:
Chemical Exposures:
-
Limit exposure to endocrine-disrupting chemicals (EDCs):
-
BPA (Bisphenol A) in plastics: Use glass or stainless steel containers
-
Pesticides: Choose organic produce when possible
-
Industrial pollutants: Minimize occupational exposure when feasible
-
Heavy metals: Reduce exposure through diet and environmental awareness
-
Heat Management:
-
Avoid hot tubs and saunas, especially regularly (limit to <30 minutes monthly if at all)
-
Discontinue hot-water baths for extended periods
-
Choose loose-fitting underwear (boxers) over tight briefs
-
Avoid placing laptops directly on your lap; use a desk or cooling pad
-
Minimize heated car seat use for extended periods
-
Limit occupational heat exposure where possible
-
Avoid prolonged sitting; take regular breaks and move around
Occupational Considerations:
-
Welders, bakers, foundry workers, and those exposed to manual work in tropical climates should take extra precautions
-
Protective equipment and scheduled breaks can help mitigate heat exposure
Lifestyle Choices:
-
Maintain a healthy weight
-
Avoid recreational drug use
-
Limit alcohol consumption
-
Avoid smoking
-
Minimize stress
Advanced Semen Parameters and Modern Assessment Tools
Sperm DNA Fragmentation (Sperm DNA Integrity)
Traditional semen analysis examines concentration, motility, and morphology, but sperm DNA fragmentation index (DFI) has emerged as an important marker of fertility potential. DFI measures the percentage of sperm with fragmented DNA, which can impact embryo development, implantation, and miscarriage rates.
-
Normal DFI: <15–20% (varies by laboratory)
-
Borderline DFI: 20–30%
-
High DFI: >30%
DNA Damage and Reproductive Outcomes:
High sperm DNA fragmentation is associated with:
-
Reduced conception rates in natural intercourse
-
Lower fertilization rates in assisted reproduction
-
Higher miscarriage rates
-
Increased risk of birth defects
-
Lower pregnancy rates in both IUI and IVF/ICSI cycles
Causes of Elevated DFI:
-
Oxidative stress (most common cause)
-
Varicocele
-
Smoking
-
Heat exposure
-
Advanced age (>40 years)
-
Infections and inflammation
-
Certain medications
-
Lifestyle factors
Testing and Improvement: Men with elevated DFI should work with specialists to address underlying causes (oxidative stress, varicocele repair, etc.) through lifestyle modifications, antioxidant supplementation, or medical treatment.
Advanced Diagnostics for Male Infertility
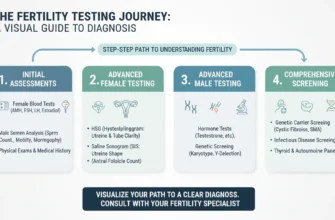
When standard semen analysis reveals abnormalities or when infertility persists despite normal basic parameters, specialists may recommend:
Hormone Testing (Reproductive Hormone Profile):
-
FSH, LH, and testosterone levels to assess hypothalamic-pituitary-gonadal axis function
-
TSH and thyroid hormones to rule out thyroid dysfunction
-
Helps distinguish between primary and secondary hypogonadism
Sperm DNA Fragmentation Analysis:
-
Measures the level of damaged DNA within sperm using techniques like TUNEL or SCSA
-
Important for predicting success with assisted reproductive techniques
Testicular Biopsy or Testicular Sperm Extraction (TESE/microTESE):
-
For men with non-obstructive azoospermia or very low sperm counts
-
Allows retrieval of sperm directly from testicular tissue for ICSI
Genetic Testing:
-
Karyotyping to screen for chromosomal abnormalities (Klinefelter syndrome, etc.)
-
Y-chromosome microdeletion testing for azoospermia factor deletions
-
CFTR gene testing for cystic fibrosis-related azoospermia
Scrotal Ultrasound:
-
Detects varicocele, structural abnormalities, or signs of testicular disease
These advanced tools help create a more complete clinical picture of fertility potential and guide targeted treatment strategies.
When to Seek Professional Fertility Guidance
Recognizing When to Consult a Fertility Specialist
It is generally recommended to consult a fertility specialist:
-
After one year of regular, unprotected intercourse without conception (or 6 months if female partner is >35 years old)
-
If there is a known risk factor, such as:
-
History of reproductive health issues
-
Previous surgeries in the genital area
-
Diagnosed medical condition affecting fertility (diabetes, testicular disease, etc.)
-
Smoking, alcohol abuse, or other lifestyle risk factors
-
Known environmental exposures
-
Family history of infertility
-
Advanced paternal age (>40 years)
-
A fertility specialist can conduct a thorough evaluation, including detailed semen analysis, hormonal profiling, and specialized testing, to guide appropriate next steps.
Treatment Options for Male Infertility
Treatment depends on the underlying cause:
Lifestyle and Dietary Modifications:
-
The foundation for improving sperm quality
-
Results visible in 2–3 months; full benefits after 74 days (complete spermatogenesis cycle)
Medical Management:
-
Antioxidant Supplementation: Vitamins C and E, zinc, selenium, CoQ10, and L-carnitine have shown promise in improving semen parameters and reducing sperm DNA fragmentation
-
Hormone Therapy: For hormonal imbalances (FSH, hCG, or testosterone therapy)
-
Infection Treatment: Antibiotics for reproductive tract infections
-
Medication Adjustments: Discontinuing medications that impair fertility
Surgical Options:
-
Microsurgical Varicocelectomy: For varicocele-related infertility, improving semen parameters in 60–80% of patients
-
Surgical Reconstruction: For obstructive azoospermia (vasovasostomy, vasoepididymostomy)
-
Testicular Sperm Extraction (TESE): For non-obstructive azoospermia
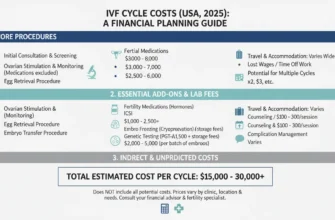
Assisted Reproductive Technologies (ART):
-
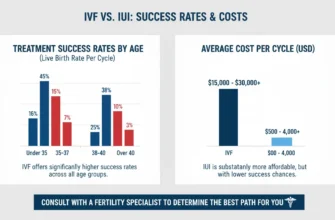
Intrauterine Insemination (IUI): Placing washed, concentrated sperm directly into the uterus. Success rates: 10–20% per cycle
-
In Vitro Fertilization (IVF): Fertilizing eggs in the laboratory, with embryos transferred to the uterus. Success rates: 30–50% per cycle (age-dependent)
-
Intracytoplasmic Sperm Injection (ICSI): Injecting a single healthy sperm directly into an egg, bypassing many natural barriers. Highly effective for severe male factor infertility. ICSI outcomes in IVF/ICSI cycles show live birth rates of 30–35% for women under 35 years
-
Testicular Sperm Extraction with ICSI: For men with non-obstructive azoospermia or failed ejaculation
Microelectronic Advances:
Modern techniques like testicular organoid development and Virtual Azoospermia classification systems are emerging research areas that may offer future treatment options.
The Recovery Timeline: When to Expect Improvements
A critical concept in male fertility: Improvement takes time. Since sperm take approximately 74 days to develop from spermatogonial stem cells to mature spermatozoa, the positive changes you make today will be reflected in the health of sperm produced over the next 2.5–3 months.
This timeline applies to:
-
Lifestyle modifications: Full benefits visible after 74 days
-
Smoking cessation: Sperm quality begins improving within 2–3 months; full recovery takes 6–12 months
-
Heat exposure avoidance: Improvement within 4–12 weeks after cessation
-
Antioxidant supplementation: Benefits typically visible after 3–6 months of consistent use
-
Varicocele repair: Improvement in DFI visible by 3–6 months post-surgery; continued improvement to 12 months
Empowering Your Journey to Parenthood
Taking a Proactive Approach to Male Fertility and Reproductive Function
Understanding your sperm health is an empowering step on the journey to parenthood. Rather than viewing fertility as beyond your control, recognizing the impact of diet, lifestyle, environmental factors, and medical conditions allows you to take proactive, evidence-based measures to enhance your reproductive potential. A semen analysis is not a final verdict but a starting point—a valuable piece of data that can guide you toward making positive changes to improve your sperm quality and fertility outcomes.
The Continuous Path to Optimal Sperm Quality
Improving sperm quality is not a one-time fix but a continuous process requiring commitment and consistency. By investing in a healthier lifestyle, optimizing your diet, managing stress, avoiding environmental hazards, and addressing medical issues, you are investing in your future family and creating the best possible biological foundation for conception and healthy embryo development through the blastocyst stage.
Final Encouragement
If you are concerned about your fertility or male infertility risk factors, the most important step is to seek professional guidance. A conversation with a fertility specialist or urologist can provide clarity, direction, and a personalized plan tailored to your specific situation. Male factor infertility affects millions of men worldwide, and numerous effective treatments and strategies are available. By combining medical expertise with proactive lifestyle management and evidence-based interventions, you can significantly improve your sperm quality, optimize your reproductive health, and move forward on your path to parenthood with confidence and hope.
Remember: You are not alone. Infertility is a medical condition affecting approximately 1 in 6 couples worldwide, with male factors contributing significantly. With proper evaluation, targeted treatment, and lifestyle optimization, most men can improve their fertility outcomes and achieve their family-building goals.