Recurrent Miscarriage Explained: Causes, Diagnosis, and Average Rates Every Woman Should Know
A pregnancy loss is a deeply personal and often devastating experience. When it happens repeatedly, the emotional weight can feel overwhelming, leaving women and their partners grappling with grief, confusion, and anxiety about the future. This journey, known as recurrent miscarriage or recurrent pregnancy loss (RPL), is more than just a series of isolated events; it’s a distinct medical condition that warrants investigation and care. Understanding the potential causes, the diagnostic process, and the actual statistical realities can empower you to navigate this challenging path with clarity and hope. This article explains the essential information every woman should know about recurrent miscarriages.
Understanding Recurrent Miscarriage: What It Is and Why It Matters
Navigating the aftermath of a single miscarriage is difficult enough, but facing multiple losses requires a specialized level of understanding and medical support. Recognizing what constitutes recurrent pregnancy loss and acknowledging its profound impact is the first step toward finding answers and effective care.
Defining Recurrent Pregnancy Loss (RPL)
Recurrent pregnancy loss (RPL) is a condition distinct from early pregnancy loss or sporadic miscarriage. While definitions have historically varied, the American Society for Reproductive Medicine (ASRM) now defines RPL as the loss of two or more pregnancies, while the Royal College of Obstetricians and Gynaecologists defines it as three or more consecutive losses. These must be clinical pregnancy losses—meaning they were confirmed by ultrasound or pathological examination, not just a positive urine pregnancy test. Most of these miscarriages occur within the first trimester. This updated ASRM definition allows for earlier investigation, providing couples with the chance to identify underlying issues sooner. The European Society of Human Reproduction and Embryology (ESHRE) in their 2023 guidelines adopted the two-loss definition.
It is important to distinguish between recurrent pregnancy loss and isolated miscarriages. About 15-25% of all clinically recognized pregnancies result in loss, but only approximately 1-5% of women experience two or more losses.
The Emotional and Psychological Impact of Recurrent Miscarriages
The impact of RPL extends far beyond the physical experience. Each spontaneous pregnancy loss brings a renewed cycle of grief, anxiety, and often a sense of failure or isolation. Couples may feel hesitant to share their news or experience anticipatory anxiety with subsequent pregnancies. This emotional toll can strain relationships and impact mental well-being. It is crucial to acknowledge that this grief is valid and seeking psychological support from therapists, support groups, or trusted loved ones is a vital part of the healing process.
When to Seek Specialized Care for Recurrent Miscarriage
If you have experienced two or more pregnancy losses, it is time to seek a consultation with a healthcare provider, preferably a reproductive endocrinologist or a maternal-fetal medicine specialist. These experts are trained to conduct a thorough investigation into the complex causes of recurrent miscarriage. An early and comprehensive evaluation is key to identifying treatable conditions that could improve your chances of a successful future pregnancy.
The Complex Landscape of Causes: Why Recurrent Miscarriages Happen
The reasons behind recurrent pregnancy loss are multifaceted, often involving a combination of factors. While in some cases a clear cause cannot be found, a systematic investigation can uncover issues related to genetic testing, anatomy, hormones, and more.
Genetic and Chromosomal Factors: The Blueprint of Life
The most common cause of sporadic, first-trimester miscarriage is a random chromosomal abnormality in the embryo. This means the embryo received too many or too few chromosomes at conception, making it non-viable. A condition called trisomy 16 is the most common single chromosome abnormality found in miscarriages. While often a matter of chance, this can become a recurrent issue.
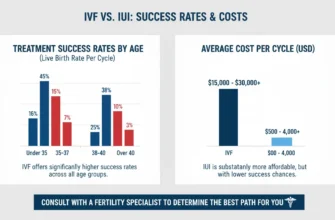
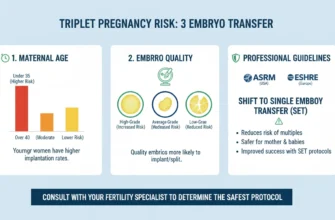
In about 2-5% of couples with RPL, one partner carries a “balanced chromosome translocation,” where a piece of one chromosome has attached to another. This is also known as a balanced reciprocal translocation or Robertsonian translocation. While this doesn’t affect the parent’s health (the parent’s karyotype is balanced), it can lead to an embryo with an incorrect amount of genetic material, resulting in miscarriage. Partners of translocation carriers have approximately a 50% risk of producing chromosomally abnormal embryos and a higher risk of miscarriage. Carrier screening can identify these carriers. When a balanced translocation is identified, preimplantation genetic diagnosis (PGD) or preimplantation genetic testing (PGT) can help select chromosomally normal embryos during In Vitro Fertilization (IVF).
Testing the pregnancy tissue or products of conception from a miscarriage can provide valuable information. If the tissue shows a chromosomal abnormality, it confirms the reason for that specific loss. If the tissue is chromosomally normal, it directs the investigation toward other maternal or paternal causes.
Uterine Abnormalities: The Womb’s Structure
The structure and health of the uterus are critical for an embryo to implant and grow. Anatomic abnormalities, present in about 10-15% of women with RPL, can interfere with this process. These include:
Congenital Anomalies: Issues like a septate uterus (a wall of tissue dividing the uterus) or a bicornuate uterus can affect implantation and blood supply. Women with a septate uterus have particularly elevated miscarriage rates (approximately 44.3% in some studies). A T-shaped uterus is another congenital anomaly that may increase miscarriage risk.
Acquired Problems: Uterine fibroids, especially those inside the uterine cavity, or polyps can disrupt the lining. Scar tissue (adhesions) from previous surgery, dilation and curettage (D&C), or infections can also pose a problem.
Cervical Insufficiency: A weakened cervix (also called cervical incompetence) that begins to dilate prematurely can lead to second-trimester loss. Almost 25% of second-trimester miscarriages are due to cervical insufficiency. This condition is typically diagnosed through transvaginal ultrasound or ultrasound scan and can be managed with cervical cerclage (stitching) or vaginal progesterone in subsequent pregnancies.
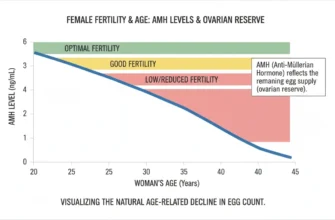
Maternal Age and Ovarian Reserve
Maternal age is one of the most significant risk factors for pregnancy loss. According to RCOG guidelines, age-related miscarriage risk ranges from 13% in women ≤19 years old to 93% in women ≥45 years old. Women over 35 years have particularly elevated miscarriage risk. Ovarian reserve tests can provide insight into the quantity and quality of remaining eggs, which naturally declines with age.
Hormonal and Endocrine Imbalances: Regulating Pregnancy
Proper hormonal balance is essential for maintaining a healthy pregnancy. Several endocrine disorders can contribute to recurrent miscarriages.
Thyroid Dysfunction: Thyroid Stimulating Hormone (TSH) abnormalities, particularly hypothyroidism and the presence of thyroperoxidase antibodies, are strongly linked to pregnancy loss. Thyroid disorders should be screened and appropriately managed.
Diabetes: Uncontrolled diabetes, with high blood sugar levels, can be harmful to a developing embryo.
Polycystic Ovary Syndrome (PCOS): Women with Polycystic Ovarian Syndrome (PCOS) have 49-53% higher odds of miscarriage compared to women without PCOS, independent of age, fertility treatment type, and obesity. The mechanism may involve hormonal imbalances and compromised endometrial receptivity.
Other Hormonal Issues: Elevated prolactin levels or problems with progesterone can impact the uterine lining and its ability to support a pregnancy. The concept of Luteal Phase defect has historically been proposed but remains controversial and is not routinely tested according to current guidelines.
Autoimmune and Immunological Factors: The Body’s Defense System
In some cases, the mother’s immune system may mistakenly attack the developing pregnancy. The most well-understood of these conditions is Antiphospholipid Syndrome (APS), also called antiphospholipid antibody syndrome.
Antiphospholipid Syndrome (APS): In APS, the body produces antibodies that increase the risk of blood clots. These tiny blood clots can form in the placenta, cutting off vital nutrients and oxygen to the embryo and leading to miscarriage. APS accounts for approximately 8-42% (mean 15%) of RPL cases and is the most clearly defined autoimmune cause of RPL. With proper treatment, pregnancy success rates have improved from 20% before 1990 to 70-80% today. At least 15% of recurrent miscarriages occur as a result of APS.
Antinuclear Antibodies (ANA): Some research suggests that women with positive ANA tests may have increased miscarriage risk, though this remains an area of investigation and debate within the medical community.
Uterine Natural Killer Cells: Research continues to explore the role of Uterine natural killer cells and other potential immunological factors in RPL, but these remain areas of ongoing research.
Blood Clotting Disorders (Thrombophilias): Impacting Placental Blood Flow
Beyond APS, inherited thrombophilias are genetic conditions that make a person’s blood more likely to clot. While the link between inherited thrombophilias and early miscarriage is less definitive than with APS, they can contribute to later pregnancy complications by impairing placental blood flow. Testing for these is often part of a comprehensive RPL workup, though current major guidelines do not routinely recommend screening for inherited thrombophilias in all couples with RPL.
Male Factor Contributions: Beyond the Egg
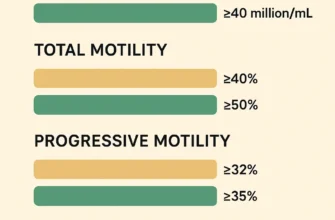
Historically, the focus of miscarriage research has been on the female partner, but emerging evidence highlights the importance of the biological father and male factor fertility. High rates of DNA fragmentation in sperm—damage to the genetic material within the sperm—have been linked to poor embryo quality and an increased risk of miscarriage. Research shows that over 85% of men whose partners had recurrent miscarriages had high sperm DNA damage. This is an area of ongoing research, and evaluating sperm health can be a valuable component of an RPL investigation.
Lifestyle and Environmental Factors: Modifiable Risks
Certain lifestyle choices and environmental exposures can increase the risk of miscarriage.
Smoking is a significant factor, as it damages both eggs and sperm and restricts blood flow to the uterus. Smoking is associated with reduced live birth rates.
Excessive alcohol consumption, illicit drug use, and high caffeine intake have also been associated with higher rates of pregnancy loss. Specifically, consuming more than 3 cups of coffee per day or 3-5 alcoholic drinks per week is associated with increased miscarriage risk.
Obesity can contribute to hormonal imbalances and inflammation, further elevating the risk.
Stress and psychological factors have been investigated, but current evidence does not establish stress as a direct cause of pregnancy loss, though it may exacerbate other conditions.
Infectious and Other Factors
While historically chronic endometritis (chronic inflammation of the uterine lining) was thought to contribute to RPL, current evidence is limited. Routine screening for bacterial vaginosis or endocervical infections is not recommended for all RPL patients.
Unexplained Recurrent Miscarriage: When No Clear Cause Is Found
After a complete evaluation, up to 50-75% of couples experiencing recurrent pregnancy loss will have no definitive cause identified. This “unexplained recurrent miscarriage” diagnosis can be frustrating, but it is not without hope. Even without a specific treatment, the prognosis for a future successful pregnancy remains high for these couples, often with supportive care and close monitoring.
Navigating the Diagnostic Journey: Finding Answers
The goal of a diagnostic workup for RPL is to systematically investigate the potential causes to guide treatment and improve the chances of a future healthy pregnancy.
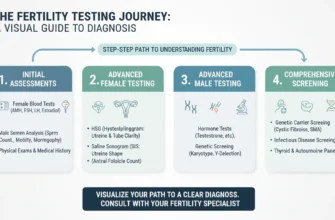
The Initial Consultation: Comprehensive Medical History and Pelvic Exam
Your journey will begin with a thorough discussion of your medical, surgical, and family history, as well as details about your previous pregnancies and their outcomes. A physical and pelvic exam will also be performed to check for any obvious physical abnormalities.
Blood Tests: A Window into Your Health
A series of blood tests provides crucial information about your health. These typically include:
Hormone Levels and Thyroid Function: To check for thyroid disorders, diabetes, and other endocrine imbalances. TSH and thyroperoxidase antibodies should be measured.
Autoimmune Screening: To test for antiphospholipid antibodies associated with Antiphospholipid Syndrome. Testing includes lupus anticoagulant, anticardiolipin antibodies, and anti-β2-glycoprotein I antibodies.
Karyotyping: A genetic test for both partners to look for chromosomal issues like balanced chromosome translocations. Karyotype analysis can identify carriers who may benefit from genetic counseling.
Thrombophilia Panel: To screen for inherited blood clotting disorders (though routine screening is not universally recommended).
Blood Type and Rhesus Factor: RH Factor status should be determined for pregnancy management and prevention of hemolytic disease of the newborn.
Uterine Evaluation: Assessing the Womb’s Environment
Imaging studies are essential for evaluating the structure of the uterus. Common methods include:
Transvaginal Ultrasound: A simple, non-invasive way to get a clear picture of the uterus and ovaries. A 3D ultrasound can provide even more detail about the uterine shape.
Hysterosalpingogram (HSG): An X-ray procedure where dye is injected through the cervix to outline the uterine cavity and check if the fallopian tubes are open. This test can reveal structural abnormalities and tubal patency.
Saline Infusion Sonogram: Also called saline sonogram or saline ultrasound, this involves injecting sterile saline into the uterus during ultrasound to better visualize the uterine cavity and identify fibroids or polyps.
Hysteroscopy: A procedure where a thin, lighted camera is inserted into the uterus to directly visualize and, if necessary, treat issues like fibroids, polyps, or a septate uterus.
Genetic Testing of Miscarriage Tissue (Products of Conception)
If possible, testing the tissue from a future miscarriage can be incredibly informative. Chromosome testing of pregnancy tissue or products of conception can identify chromosome abnormalities. If the tissue shows a chromosomal abnormality, it confirms the reason for that specific loss. If the tissue is chromosomally normal, it directs the investigation toward other maternal or paternal causes.
Miscarriage tissue testing, also known as POC testing (products of conception testing), uses advanced genetic testing techniques to analyze DNA and determine if the miscarriage was caused by chromosome aneuploidy.
Additional or Specialized Testing
Depending on your history, your doctor may recommend further tests.
Ovarian Reserve Tests: Ovarian reserve testing can provide insight into the quantity and quality of your remaining eggs. Tests may include Anti-Müllerian Hormone (AMH) measurement and antral follicle count (AFC).
Sperm DNA Fragmentation Test: A sperm DNA fragmentation test may be suggested to evaluate the male factor contribution.
Adenomyosis Evaluation: Recent guidelines have added recommendations for assessing adenomyosis (abnormal endometrial tissue growth into the myometrium) in women with RPL, as it may affect pregnancy outcome.
Treatment Strategies and Management Options: Tailored Approaches
Once a diagnosis is made, treatment is tailored to the specific cause. Even in unexplained cases, supportive strategies can improve outcomes.
Treatments for Genetic Causes
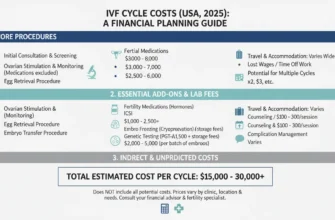
If a balanced translocation is found, the primary option to reduce miscarriage risk is In Vitro Fertilization (IVF) with Preimplantation Genetic Testing (PGT), also called preimplantation genetic diagnosis (PGD). This allows for the screening of embryos for the correct number of chromosomes before one is transferred to the uterus. IVF with genetic testing can significantly improve outcomes for carriers of balanced translocations.
Addressing Uterine Abnormalities
Many structural issues within the uterus can be corrected with minimally invasive surgery. A hysteroscopy can be used to remove a septate uterus, fibroids, or polyps, restoring a normal uterine cavity and improving the environment for a pregnancy to thrive. For women with cervical insufficiency, cervical cerclage (placement of a stitch to support the cervix) or cervical surgery can be offered in subsequent pregnancies.
Managing Hormonal and Endocrine Imbalances
Hormonal issues are typically managed with medication.
Thyroid Disorders: Thyroid hormone replacement can correct hypothyroidism.
Diabetes and Insulin Resistance: Medications like metformin can help control blood sugar and insulin resistance.
Progesterone Supplementation: Low-dose progesterone or progesterone therapy is sometimes used in early pregnancy to support the uterine lining, though research on their effectiveness for all RPL cases is mixed. The PROMISE trial showed that vaginal progesterone at 400 mg daily increased the live birth rate by only 3% (not statistically significant). However, progesterone may be beneficial for patients with specific luteal phase abnormalities or certain immunological issues.
Therapies for Autoimmune and Clotting Disorders
For women diagnosed with Antiphospholipid Syndrome (APS), the standard treatment to prevent blood clots and support the pregnancy is a combination of low-dose aspirin (75-150 mg daily) and an injectable blood thinner called heparin (unfractionated heparin or low-molecular-weight heparin). This therapy significantly improves the live birth rate for affected women, with success rates of 70-80%. Aspirin plus unfractionated heparin reduces the miscarriage rate by 54% compared to aspirin alone.
For women with other autoimmune markers (such as positive ANA antibodies), emerging research suggests that combination therapy with low-dose aspirin, glucocorticoids, and sometimes intravenous immunoglobulin may be beneficial, though more research is needed.
Lifestyle Modifications and Supportive Care
Addressing modifiable risk factors is a crucial step. This includes:
-
Stopping smoking
-
Reducing alcohol and caffeine intake
-
Achieving a healthy weight
-
Regular exercise
-
Stress management and psychological support
Supportive care, which involves early monitoring with ultrasound scans and bloodwork in a subsequent pregnancy, can provide reassurance and has been shown to improve outcomes even in unexplained cases. Some centers offer dedicated early pregnancy loss clinics where women receive frequent monitoring and specialized support.
Approaches for Unexplained Recurrent Miscarriage
For the many couples with unexplained recurrent miscarriage, the focus is on optimizing overall health and providing strong emotional and medical support during the next pregnancy. While frustrating, it is important to remember that the majority of these couples will go on to have a successful pregnancy without a specific intervention.
Expectant management (allowing natural conception to proceed with supportive care) has been shown to result in live birth rates of 60-70% for couples with unexplained RPL, demonstrating that the natural prognosis is often favorable.
Understanding the Odds: Average Rates and Prognosis for Future Pregnancies
While the experience of recurrent miscarriage can feel isolating, understanding the statistics can provide valuable perspective and a reason for optimism.
General Miscarriage Rates vs. Recurrent Miscarriage Incidence
Miscarriage is common, with an estimated 15-25% of all clinically recognized pregnancies ending in loss, most in the first trimester. Recurrent pregnancy loss, defined as two or more losses, is much less common, affecting approximately 1-5% of women. The incidence of early loss of pregnancy specifically affecting couples is estimated at 1-2%. While this percentage seems small, it represents a significant number of families facing this challenge.
The risk of experiencing another miscarriage increases with each prior loss: after one miscarriage, the risk of another is 12-20%; after two miscarriages, the risk rises to 29%; and after three miscarriages, the risk reaches 36%.
Chances of Success After Recurrent Pregnancy Loss
Perhaps the most important statistic is the chance of future success. Even after two or three miscarriages, the prognosis is often very good.
For couples with unexplained RPL, the chance of having a successful live birth in their next pregnancy is estimated to be between 60-70%. Large cohort studies show that approximately 77% of women with RPL who have a subsequent pregnancy will conceive, and among those pregnancies, the live birth rate is approximately 63%.
Cumulative live birth rates (multiple pregnancy attempts) are even higher, with approximately two-thirds to three-quarters of women with recurrent miscarriage achieving at least one live birth within 5 years of their first consultation at a specialized clinic.
When a specific cause is identified and treated—such as a septate uterus that is removed via hysteroscopic surgery or an autoimmune disorder managed with aspirin and heparin—the live birth rates can be even higher, sometimes exceeding 70-80%.
Maternal age significantly affects prognosis. Women aged 40 and older have a live birth rate of approximately 44% after RPL, compared to higher rates in younger women. Secondary RPL (pregnancy loss after a previous live birth) tends to have a somewhat more favorable prognosis than primary RPL.
This data underscores a powerful message of hope: a history of loss does not preclude a future of family.
Psychological Support and Care Organization
The emotional impact of recurrent miscarriage is profound and should not be underestimated. Psychological support should be an integral part of care for all couples experiencing RPL. This may include:
-
Individual or couple counseling
-
Support groups for women’s health issues
-
Access to mental health professionals experienced in reproductive trauma
-
Information and education about the condition
-
Genetic counseling when appropriate
Care should be organized through specialized clinics staffed by OB/GYN specialists experienced in recurrent pregnancy loss management, ideally in collaboration with reproductive endocrinologists and other specialists. Organizations such as the American College of Obstetricians and Gynecologists (ACOG) and the American Society of Reproductive Medicine (ASRM) provide guidelines to support comprehensive care.
Conclusion
Recurrent miscarriage is a complex and emotionally taxing condition, but it is not an endpoint. Through comprehensive medical investigation, it is often possible to identify underlying causes related to genetics, uterine anatomy, chromosomal abnormalities, hormones, and the immune system. This diagnostic journey provides the foundation for targeted treatments, from corrective surgery to medication and lifestyle changes, that can significantly improve the chances of a healthy pregnancy.
Even when no clear cause is found, the data shows that hope is far from lost. By seeking specialized care, advocating for a thorough evaluation including karyotype analysis and chromosome testing, and embracing supportive therapies, women and their partners can navigate this difficult path and move with confidence toward their goal of building a family.
Resources such as the Miscarriage Support Tool, Miscarriage Research Centre, information from Harvard Health Publishing, and guidelines from the American Society of Reproductive Medicine and the European Society of Human Reproduction and Embryology can provide additional education and support. The Washington University Fertility and Reproductive Medicine Center and similar institutions continue to advance understanding through research published in journals like the Cochrane Library to improve outcomes for couples facing this challenge.