The Essential Guide: Top Vitamins for Women’s Fertility & Conception Success
Nurturing Your Fertility Journey with Nutrition
Embarking on the path to parenthood is a profound journey, and preparing your body for conception is a powerful first step. While many factors influence fertility, nutrition plays a foundational role in creating an optimal environment for pregnancy. The vitamins, minerals, and nutrients you consume directly impact your reproductive health, from hormonal balance to egg quality. This guide is designed to demystify the science of fertility nutrition, providing a clear roadmap to the essential vitamins that can support your journey to conception success.
The Power of Proactive Nutrition for Conception
Proactive nutrition isn’t about a last-minute diet change; it’s about building a nutrient-rich foundation to support every stage of the reproductive process. The health of your eggs, the regularity of your menstrual cycle, and the uterine environment are all influenced by your dietary intake. By focusing on key nutrients before you even start trying to conceive, you are not only enhancing your female fertility but also preparing your body to nurture a healthy pregnancy from the very first moments.
Research demonstrates that women attempting conception benefit significantly from adequate micronutrient status. Studies show that over 90% of women in high-income countries have marginal or low concentrations of at least one critical vitamin during the preconception period, underscoring the widespread need for targeted nutritional support.
What This Guide Will Cover: Diet First, Smart Supplementation Second
Our philosophy is simple: whole foods are the primary source of essential nutrients. This guide will first explore the biological link between what you eat and your reproductive health. We will then detail the most critical vitamins and minerals, highlighting their roles and the best dietary sources. Finally, we’ll discuss how smart, targeted supplements, such as prenatal vitamins, can fill nutritional gaps and provide an extra layer of support, always emphasizing the importance of professional medical advice.
The Foundation: How Nutrients Shape Female Reproductive Health
Understanding the “why” behind fertility nutrition is crucial. Your reproductive system is a complex network of hormonal signals and cellular processes. Key nutrients act as the building blocks and fuel for this intricate system, ensuring everything functions in harmony. A deficiency in even one critical area can disrupt this delicate balance.
Understanding the Intricate Link Between Diet and Fertility
Every meal is an opportunity to nourish your fertility. The foods you choose provide the energy and raw materials needed for hormone production, egg maturation, and the development of a healthy uterine lining. Conversely, a diet lacking in essential nutrients can contribute to hormonal imbalances and ovulatory dysfunction. Research demonstrates that women whose diets have a high glycemic load are at significantly greater risk of ovulatory infertility. In a prospective study of over 18,500 women, those in the highest quintile of dietary glycemic load had nearly twice the risk of ovulatory infertility compared to those in the lowest quintile (RR 1.92, 95% CI 1.26-2.92).
Key Biological Processes Supported by Optimal Nutrition
Hormonal Regulation: Vitamins and minerals are cofactors in the synthesis of reproductive hormones like estrogen and progesterone, which govern the menstrual cycle.
Egg Quality (Oocyte Health): Antioxidants protect developing eggs from cellular damage, while other nutrients provide the energy needed for maturation.
Ovulation: A consistent supply of specific nutrients helps support the regular release of a healthy egg.
Uterine Lining Development: A nutrient-rich blood supply, supported by minerals like iron, is vital for creating a receptive endometrial lining for implantation.
Essential Vitamins & Nutrients for Fertility & Conception Success (The “Cornerstones”)
While a balanced diet is key, certain nutrients are non-negotiable standouts on the path to pregnancy. These cornerstones play pivotal roles in both preconception health and early fetal development.
Folate (Folic Acid): The Non-Negotiable for Neural Tube Development & Beyond
Folate (the natural form) and folic acid (the synthetic form used in supplements) are B-vitamins critical for preventing neural tube defects in a developing fetus. Since these defects can occur in the first few weeks of pregnancy—often before a woman knows she is pregnant—it is essential to have adequate levels before conception.
The U.S. Preventive Services Task Force (USPSTF) recommends that all persons planning to or who could become pregnant take a daily supplement containing 0.4 to 0.8 mg (400 to 800 μg) of folic acid, reaffirming this recommendation in 2023 based on high-certainty evidence of substantial net benefits. Countries with mandatory folic acid fortification have demonstrated up to 78% reductions in neural tube defect rates.
Beyond preventing birth defects, folate supports cell division and DNA synthesis, processes fundamental to healthy egg development and ovulation.
Vitamin D: The “Sunshine Vitamin” for Hormonal Balance & Egg Health
Often associated with bone health, Vitamin D also acts as a hormone that influences the reproductive system. It plays a role in regulating menstrual cycles and improving ovarian stimulation.
Research from 2023 demonstrates that vitamin D supplementation contributes to higher pregnancy and ovulation rates, and lower androgen levels in women with polycystic ovary syndrome, with improvements occurring regardless of the use of ovulation induction drugs or assisted reproductive technologies. Vitamin D deficiency is surprisingly common, with studies consistently linking low levels to adverse outcomes, including PCOS.
While sunlight is a primary source, dietary intake and supplementation are often necessary to maintain optimal levels for fertility. Vitamin D receptors are found in reproductive organs, tissues, and granulosa cells, emphasizing its crucial role in follicular development and hormone production.
Coenzyme Q10 (CoQ10): Energizing Egg Cells for Optimal Function
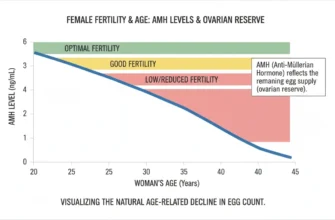
CoQ10 is a powerful antioxidant that is crucial for energy production within the mitochondria—the powerhouses of every cell, including egg cells. As women age, CoQ10 levels naturally decline, which can impact egg quality.
A landmark 2015 study published in Aging Cell demonstrated that supplementing with CoQ10 reversed age-related decline in oocyte quality and quantity in animal models. The study found that CoQ10 treatment restored normal spindle appearance and chromosomal alignment in aged oocytes, normalized metabolite production, and resulted in litter sizes similar to young animals, providing compelling evidence that “impaired mitochondrial performance created by suboptimal CoQ10 availability can drive age-associated oocyte deficits causing infertility.” Supplementing with CoQ10 can help improve mitochondrial function, providing eggs with the energy they need for successful fertilization and early embryo development.
Iron: Vital for Oxygen Transport, Ovulation & Uterine Health
Iron is essential for producing hemoglobin, the protein that carries oxygen throughout your body. An adequate iron supply ensures your reproductive organs receive the oxygen-rich blood they need to function correctly.
Iron deficiency can lead to anovulation (a lack of ovulation). Research demonstrates that women with ferritin levels below 30 ng/mL show 30-50% less ovulation, and approximately 50% of women with iron deficiency anemia report amenorrhea. A 2025 study found that treating iron deficiency with intravenous ferric carboxymaltose resulted in a 77% conception rate and 51% live birth rate among infertile women with serum ferritin ≤30 μg/L, compared to 28% miscarriage rates that fell to 13% post-treatment.
Building up iron stores before pregnancy is also crucial to support the increased blood volume required and prevent anemia.
Iodine: Essential for Thyroid Health and Reproductive Function
Iodine is a critical component of thyroid hormones, which regulate metabolism and play a direct role in ovarian function. A healthy thyroid is essential for regular ovulation and overall reproductive health.
Iodine deficiency can disrupt the menstrual cycle and negatively impact fertility. Research from the National Institutes of Health found that women with moderate to severe iodine deficiency had a 46% lower chance of getting pregnant each cycle compared to women with normal iodine levels. Making it a key nutrient to monitor during the preconception period.
Key Supporting Nutrients for Enhanced Fertility (The “Game-Changers”)
Beyond the cornerstones, a supporting cast of nutrients can further optimize your reproductive health, addressing everything from inflammation to cellular protection.
Omega-3 Fatty Acids (DHA & EPA): Anti-Inflammatory & Hormonal Support
Omega-3s, particularly DHA and EPA found in fatty fish, are known for their potent anti-inflammatory properties. They help regulate hormones, increase blood flow to the uterus, and may improve egg quality. By reducing systemic inflammation, omegas create a more favorable environment for conception and a healthy pregnancy.
A 2022 study examining women undergoing assisted reproductive technology found that those in the highest quartile of EPA+DHA intake had nearly twice the probability of live birth (0.54) compared to women in the lowest quartile (0.36), with inverse relationships also observed for pregnancy loss. In natural fertility, women taking omega-3 supplements were almost twice as likely to conceive spontaneously in a given menstrual cycle compared to those not taking supplements.
Zinc: A Crucial Mineral for Ovarian Function & Cell Division
Zinc is involved in hundreds of enzymatic reactions in the body, including many related to fertility. It is vital for egg maturation and plays a role in maintaining regular menstrual cycles.
During fertilization, a “zinc spark” is released, a crucial event for the egg to properly begin dividing into an embryo. Adequate intracellular zinc in oocytes maintains meiotic arrest at prophase I until the germ cell is ready to undergo maturation; dietary zinc deficiency disrupts maturation and reduces oocyte quality.
Selenium: Powerful Antioxidant for Egg Protection
Selenium is a trace mineral that functions as a powerful antioxidant, protecting egg follicles from oxidative stress and DNA damage. This protection is critical for preserving egg quality. Research shows that women with higher selenium levels tend to have better oocyte quality and higher fertilization rates during IVF treatments.
Selenium also supports thyroid function, working in tandem with iodine to ensure proper hormonal balance for reproductive health.
B Vitamins (B6, B12, Choline): Homocysteine, Hormones & Early Development
Beyond folate (B9), other B vitamins are essential. Vitamin B6 helps regulate hormones and blood sugar. Vitamin B12 is crucial for red blood cell formation and neurological function.
A landmark 2023 study from the University of Southampton examining over 1,700 pregnant women from high-income countries (UK, New Zealand, Singapore) found that 90% had marginal or low concentrations of one or more critical vitamins during the preconception period, with B12, B6, D, folic acid, and riboflavin being particularly insufficient. The study noted that B12 deficiency markers were present in nearly half of participants, while most developed B6 deficiency during late pregnancy.
Research demonstrates that poor vitamin B6 status decreases the probability of conception and contributes to the risk of early pregnancy loss, with women in the highest quartiles of B6 status showing higher adjusted conception rates (HR=2.2-2.4) and lower risks of early pregnancy loss.
Choline is also vital for fetal brain development. It plays a critical role in neural tube formation and cognitive development. A meta-analysis found that low maternal choline intake was associated with a 36% higher odds of neural tube defects, with risks potentially reaching 2.36-fold in some populations. Additionally, higher maternal choline levels during pregnancy were associated with better performance in infant inhibition tests and behavioral regulation at 3-month follow-ups.
Inositol (Myo-inositol): A Standout for Ovulatory Health, Especially with PCOS
Inositol, particularly myo-inositol, is a vitamin-like compound that has shown significant promise in improving ovarian function and restoring menstrual regularity, especially for women with Polycystic Ovary Syndrome (PCOS). It helps improve insulin sensitivity, which can in turn help balance hormones and promote ovulation.
Studies demonstrate that myo-inositol supplementation may lead to increased ovulation rates and improved pregnancy outcomes in women with PCOS. After 12 weeks of therapy, participants experienced significant reductions in plasma LH and insulin levels, with most women regaining regular menstrual cycles and spontaneous ovulation.
Vitamin C & E: Synergistic Antioxidants for Cellular Health
Vitamin C and Vitamin E work together as a powerful antioxidant team. Vitamin C regenerates Vitamin E, enhancing its ability to protect cells from damage. Research has associated higher intakes of Vitamin C with a lower risk of female infertility.
This duo helps protect egg and sperm DNA, supports the luteal phase of the menstrual cycle, and enhances overall cellular health within the reproductive system. A meta-analysis found that adequate dietary antioxidant intake—including vitamins C and E—was associated with reduced female infertility risk.
Navigating Prenatal Vitamins & Supplementation Wisely
While a nutrient-dense diet is the goal, supplements can provide a crucial safety net, ensuring you get consistent, optimal levels of key nutrients for conception.
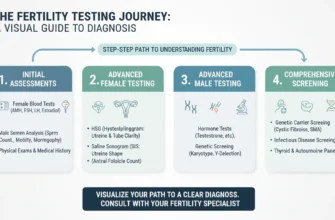
When to Start: Proactive Supplementation Before Conception
Ideally, you should start taking a prenatal vitamin at least three months before you begin trying to conceive. This period allows your body to build up stores of essential nutrients, particularly folic acid and iron, ensuring they are readily available from the moment of conception for healthy fetal development.
What to Look For in a Quality Prenatal Vitamin: Comprehensive Coverage
A good prenatal vitamin should contain adequate amounts of folic acid (at least 400-800 mcg), iron, vitamin D, iodine, and choline. Look for products that use bioavailable forms of nutrients (like methylfolate instead of folic acid for some individuals) and are third-party tested for purity and potency.
The University of Southampton study found that supplementation in amounts available in over-the-counter supplements substantially reduces the prevalence of vitamin deficiency markers, with greater maternal plasma vitamin B12 maintained during the recommended lactational period.
The Importance of Consulting Your Healthcare Provider (OB/GYN, Fertility Specialist)
Before starting any new supplement regimen, it is essential to consult with your doctor or a fertility specialist. They can assess your individual needs through blood work, review your health history, and recommend a personalized plan. This ensures you are taking the right nutrients in the right amounts for your specific situation.
Avoiding Over-Supplementation and Potential Risks
More is not always better. Excessively high doses of certain fat-soluble vitamins (like A and D) can be toxic. Adhering to the recommended daily allowances and following your healthcare provider’s guidance is the safest and most effective approach to supplementation for fertility.
Additionally, emerging research suggests that excessive iodine intake may have adverse effects on fertility. Both iodine deficiency and excess can negatively impact reproductive outcomes, with optimal levels being crucial for both male and female reproductive health.
Decoding Fertility Supplements: What to Consider and What to Question
The market for fertility supplements is vast. Be critical of products that make extravagant claims. Stick to supplements with evidence-backed ingredients discussed in this guide. Focus on quality, transparency, and third-party verification rather than marketing promises. Your doctor can help you navigate these choices.
Beyond Vitamins: Integrating Diet and Lifestyle for Holistic Fertility Support
Nutrients do not work in a vacuum. True fertility enhancement comes from a holistic approach that combines a supportive diet with healthy lifestyle habits.
Building a Fertility-Friendly Diet: Practical Steps and Meal Ideas
Focus on a whole-foods diet rich in fruits, vegetables, lean proteins, healthy fats, and complex carbohydrates. The Mediterranean diet has demonstrated a strong association with improved pregnancy outcomes. A 2023 meta-analysis of 32 studies including 103,204 women found that higher Mediterranean Diet adherence was associated with reduced gestational diabetes (RR 0.74), preterm birth (RR 0.45), gestational hypertension (RR 0.71), and preeclampsia (RR 0.82).
Include leafy greens for folate, fatty fish for omega-3s, nuts and seeds for zinc and selenium, and lean meats or legumes for iron. Women following this dietary pattern showed enhanced embryo development, higher live birth rates, and reduced difficulty conceiving.
Complementary Lifestyle Pillars for Reproductive Health
Stress Management: Chronic stress can disrupt hormonal balance. Incorporate practices like yoga, meditation, or mindfulness.
Moderate Exercise: Regular physical activity improves circulation and insulin sensitivity, but avoid over-exertion, which can negatively impact ovulation.
Adequate Sleep: Aim for 7-9 hours of quality sleep per night, as it is crucial for hormone regulation and cellular repair.
Maintain a Healthy Weight: Being either underweight or overweight can affect hormone production and menstrual regularity. Research demonstrates that obesity enhances hormonal and metabolic disturbances leading to anovulation.
The Synergy of Nutrition and Lifestyle for Conception Success
The true power lies in the synergy between a nutrient-rich diet, smart supplementation, and a healthy lifestyle. Each pillar supports the others, creating a robust foundation for your reproductive health. This comprehensive approach gives your body its best possible chance for successful conception and a healthy pregnancy.
Evidence-Based Recommendations Summary
| Nutrient | Recommended Daily Intake | Key Functions | Top Dietary Sources |
|---|---|---|---|
| Folate/Folic Acid | 400-800 mcg | Neural tube development, DNA synthesis, ovulation | Leafy greens, legumes, fortified grains |
| Vitamin D | 1,000-2,000 IU (25-50 mcg) | Hormone regulation, menstrual cycle support, ovarian function | Fatty fish, egg yolks, mushrooms, sunlight |
| CoQ10 | 100-300 mg | Mitochondrial energy, egg quality, age-related decline | Meat, fish, nuts, seeds (supplementation often needed) |
| Iron | 18 mg (preconception), 27 mg (pregnancy) | Oxygen transport, ovulation, hemoglobin production | Red meat, poultry, legumes, fortified grains |
| Iodine | 150 mcg | Thyroid hormone production, ovulation, metabolism | Seafood, dairy, eggs, iodized salt |
| Zinc | 8-11 mg | Oocyte maturation, hormonal balance, zinc spark | Meat, shellfish, legumes, nuts, seeds |
| Selenium | 55 mcg | Antioxidant protection, egg health, thyroid function | Brazil nuts, seafood, meat, eggs |
| Omega-3 (DHA/EPA) | 200-300 mg | Anti-inflammatory, blood flow, hormone regulation | Fatty fish, algae supplements, walnuts |
| Vitamin B6 | 1.3-1.5 mg | Hormone regulation, homocysteine metabolism, conception | Chicken, fish, potatoes, chickpeas |
| Vitamin B12 | 2.4 mcg | Red blood cell formation, DNA synthesis, homocysteine metabolism | Meat, fish, dairy, eggs, fortified cereals |
| Choline | 400-550 mg (or higher during pregnancy) | Fetal brain development, neural tube formation | Eggs, meat, fish, legumes, Brussels sprouts |
| Myo-inositol | 2-4 g daily (for PCOS) | Insulin sensitivity, menstrual regularity, PCOS management | Fruits, nuts, legumes, whole grains |
| Vitamin C | 75-90 mg | Antioxidant, collagen production, luteal support | Citrus fruits, berries, peppers, broccoli |
| Vitamin E | 15 mg | Antioxidant, oxidative stress reduction, cell protection | Nuts, seeds, vegetable oils, leafy greens |
Conclusion
Preparing your body for pregnancy is an empowering act of self-care. By prioritizing a nutrient-dense diet and incorporating key vitamins and minerals, you can significantly enhance your fertility and set the stage for a healthy conception. The cornerstones—Folate, Vitamin D, CoQ10, and Iron—are non-negotiable, while game-changers like Omega-3s, Zinc, and B vitamins provide comprehensive support.
Remember the guiding principle: diet first, followed by smart, targeted supplementation.
Your next steps are clear: begin incorporating fertility-friendly foods into your daily meals, consider starting a high-quality prenatal vitamin, and most importantly, schedule a conversation with your healthcare provider. They can provide personalized guidance based on your unique health profile, ensuring your nutritional strategy is perfectly aligned with your goal of a successful pregnancy.
This proactive, informed approach to nutrition is one of the most impactful investments you can make in your future family’s health.
Key Statistics on Women’s Nutrient Status
-
90% of women in high-income countries have marginal or low concentrations of at least one critical vitamin during the preconception period
-
~50% of women with iron deficiency anemia report amenorrhea
-
Women with ferritin <30 ng/mL show 30-50% less ovulation
-
54% of pregnant women are deficient in choline
-
Women in the highest glycemic load quintile have 1.92 times the risk of ovulatory infertility
-
Women taking omega-3 supplements are almost 2 times more likely to conceive spontaneously
-
Mediterranean Diet followers have 45-74% reductions in adverse pregnancy outcomes
This guide is for informational purposes and should not replace professional medical advice. Always consult with your healthcare provider before starting any new supplementation regimen, especially if you have underlying health conditions or are taking medications.